Abstract
Many properties of polypropylene mesh that are causative in producing the complications that our patients are experiencing were published in the literature prior to the marketing of most currently used mesh configurations and mesh kits. These factors were not sufficiently taken into account prior to the sale of these products for use in patients. This report indicates when this information was available to both mesh kit manufacturers and the Food and Drug Administration.
Similar content being viewed by others
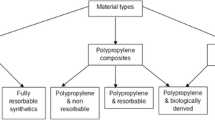
There has been a lack of dissemination of information regarding many of the characteristics of polypropylene mesh especially the many factors which are implicated in the complications that our patients experience postoperatively. The first polypropylene mesh kit cleared by the US Food and Drug Administration (FDA) for implantation was that used in the transvaginal tape (TVT®) procedure for the treatment of stress incontinence. This clearance was granted in 1998. Previously in 1996, a woven polyester mesh kit was cleared and further meshes and mesh kits meshes were granted clearance in the ensuing years. All FDA information regarding clearance for marketing dates is available at http://www.fda.gov/MedicalDevices/default.htm. I will concentrate here on those factors known to influence the behavior of mesh in vivo until 2003, when many more new mesh kits were cleared by the FDA. Heat effects and degradation will be summarized.
Relevant information has accumulated since the 1950s and was available in the medical literature for many years before FDA clearance of various meshes and mesh kits as outlined below (PP: polypropylene; SEM: scanning electron microscopy; FBGC: foreign body giant cells):
-
1953
Any implanted device must not be physically modified by tissue fluids, be chemically inert, not incite an inflammatory or foreign body cell response, be non-carcinogenic, not produce allergic reactions, stand up to mechanical stress, be fabricated in form required at low cost and be capable of sterilization [1].
-
1962
PP monofilament suture had high tensile strength, good flexibility and resistance to fatigue along with good knot retention along with being inert with excellent chemical resistance [2].
-
1967
One hundred bacteria were enough to cause infection of a multfilament suture and monofilament suture withstood infection [3].
-
1967
Monofilament suture is better than multifilament suture in wound infections [4].
-
1973
Granulation formation related to friction between tissue and implant [5].
-
1977
Immobile bacteria propagate inside multifilament suture and this plays a role in the spread of infection [6].
-
1979
Bacteria are protected in interstices of material [7].
-
1981
Bacterial adherence to multifilament suture 5-8 times greater than monofilament suture as documented with SEM [8].
-
1980
Pore size is important for tissue incorporation [9].
-
1983
Bacteria are protected in interstices from phagocytosis since leukocytes cannot readily enter the small pores of multifilament suture which supports infection and may result in sustained and prolonged infection [10, 11].
-
1983
Multifilament sutures harbor bacteria at 70 days after implantation as shown with SEM [12].
-
1984
Heat exposed PP releases biologically active degradation products affecting normal metabolic events [13].
-
1986
Degradation of PP suture known as seen with SEM [14].
-
1987
Immediately upon insertion of a mesh there is a race to the mesh surface between bacteria and host defense cells [15].
-
1991
Bacteria adhere more to hydrophobic surfaces and produce a biofilm which further protects them from phagocytosis and antibiotics [16].
-
1993
Multifilament mesh with a histiocytic reaction and unstable fixation which promotes infection [17].
-
1993
Bacteria migrate along synthetic polymeric fibers [18].
ProteGen® Sling Mesh Kit FDA Clearance Letter Dated November 15, 1996
TVT® FDA Clearance Letter Dated January 28, 1998
-
1998
Bacteria adhere to biomaterials using a biofilm [21].
-
1998
PP mesh shrinks 30-50% after 4 weeks [22].
-
1999
A multifilament mesh must be removed with infection [23].
-
1999
Surface roughness promotes wicking of bacteria [24].
-
1999
Ten bacterial colony forming units are enough to infect 15% of multifilament meshes [25].
Prolene Soft Mesh® FDA Clearance Letter Dated May 23, 2000
-
2000
Bacterial colonization found in 33% of explanted meshes [26].
IVS® FDA Clearance Letter Dated April 4, 2001
SPARC® FDA Clearance Letter Dated October 26, 2001
All Other Meshes/Kits Have FDA Clearance Letters Dated after 2001
-
2002
The extent of bacterial adherence depends on the mesh surface area. Multifilament meshes have a 205% increase in surface area compared to monofilament meshes. This may explain infection months to years after implantation [29].
-
2007
Heat sterilization causes degradation [30]. Figures 1 and 2.
Fig. 1 The control polypropylene mesh. Note the smooth surface with minimal striations as seen under SEM at 1500x. Reprinted from The American Journal of Surgery, 195(3), Kemal Serbetci et al, Effects of resterilization on mechanical properties of polypropylene meshes, pages 375–9, Copyright 2007, with permission of Elsevier and the author
Fig. 2 Degradation of polypropylene mesh after three autoclavings. Note the more pronounced irregularities with small protrusions on the surface of the polypropylene fiber as seen in SEM at 1500x. Reprinted from The American Journal of Surgery, 195(3), Kemal Serbetci et al, Effects of resterilization on mechanical properties of polypropylene meshes, pages 375–9, Copyright 2007, with permission of Elsevier and the author
-
2010
Degradation occurs in all currently used meshes [31]. Figures 3 and 4.
Fig. 3 Degradation of a non-knitted, non-woven mesh removed from a patient seen in SEM at 850x. Note the nearly completely broken fiber in the center and other degraded fibers with deep cracks in the background. Grateful acknowledgement is given to patient S. A. Y. who gave permission to reproduce this SEM
An abundance of information was available for both the FDA and mesh manufacturers prior to the FDA clearance of most meshes. Many publications detailed degradation mechanisms including heat exposure during manufacture and bacterial colonization of the polypropylene used in pelvic repair meshes.
References
Scales JT (1953) Tissue reactions to synthetic materials. Proc R Soc Med 46:647–52
Usher FC, Allen JE Jr, Crosthwait RW, Cogan JE (1962) Polypropylene monofilament: a new, biologically inert suture for closing contaminated wounds. JAMA 179:780–2
Alexander JW, Kaplan JZ, Altemeier WA (1967) Role of suture materials in the development of wound infection. Ann Surg 165:192–9
Van Winkle W, Jr HJC, Barker E, Hines D, Nichols W (1975) Effect of suture materials on healing skin wounds. Surgery 140:933–7
Homsy CA, Kent JN, Hinds EC (1973) Materials for oral implantation-biological and functional criteria. JADA 86:817–32
Blomstedt B, Osterberg B, Bergstrand A (1977) Suture material and bacterial transport. Acta Chir Scand 143:71–3
Osterberg B, Blomstedt B (1979) Effect of suture materials on bacterial survival in infected wounds. Acta Chir Scand 145:431–4
Katz S (1981) Bacterial adherence to surgical sutures: a possible factor in suture induced infections. Ann Surg 194:35–41
White RA, Hirose FM, Sproat RW, Lawrence RS, Nelson RJ (1981) Histopathologic observations after short-term implantation of two porous elastomers in dogs. Biomaterials 2:171–6
Osterburg B (1983) Influence of capillary multifilament sutures on the antibacterial action of inflammatory cells in infected wounds. Acta Chir Scand 149:751–7
Osterburg B (1983) Enclosure of bacteria within capillary multifilament sutures as protection against leukocytes. Acta Chir Scand 149:663–8
Bucknall TF (1983) The choice of suture to close abdominal incisions. Euro Surg Res 15:59–65
Frostling H, Hoff A, Jacobsson S, Pfaffii P, Vainiotalo S, Zitting A (1984) Analytical, occupational and toxicologic aspects of the degradation products of polypropylene plastics. Scand J Work Environ Health 10:163–9
Jongebloed WL, Worst JF (1986) Degradation of polypropylene in the human eye: a SEM study. Doc Ophthalmol 64:143–52
Gristina AG (1987) Biomaterial-centered infection: microbial adhesion versus tissue integration. Science 237:1588–95
Merritt K, Chang CC (1991) Factors influencing bacterial adherence to biomaterials. J Biomater Appl 5:185–203
Amid PK (1993) Biomaterials and abdominal wall hernia surgery and principles of their applications. Langenbecks Arch Chir 379:168–71
Mahmoud WM, Vieth RF, Coughlin RW (1996) Migration of bacteria along synthetic polymeric fibers. J Biomater Sci Polym Ed 7:751–2
Schraut W, Wendelgass P, Calzada-Wack J, Frankenberger M, Ziegler-Heitbrock H (1997) TNF gene expression in monocytes of low and high responder individuals. Cytokine 9:206–11
Gl B, Go PM, van Mameren H (1996) Foreign body reactions to monofilament and braided polypropylene mesh used as preperitoneal implants in pigs. Eur J Surg 162:823–5
An YH, Friedman RJ (1998) Concise review of mechanisms of bacterial adhesion to biomaterial surfaces. J Biomed Mater Res (Appl Biomater) 43:338–48
Klinge U, Klosterhalfen B, Muller M, Ottinger AP, Schumpelick V (1998) Shrinkage of polypropylene mesh in vivo: an experimental study in dogs. Eur J Surg 164:965–9
Goldstein HS (1999) Selecting the right mesh. Hernia 3:23–6
Coughlin RW, Mullen D, Brancieri M, Rezman V, Vieth RF (1999) Surface roughness enhances upward migration of bacteria on polymer fibers above liquid cultures. J Biomater Sci Polym Ed 10:827–44
Merritt K, Chang CC (1999) Tissue colonization from implantable biomaterials with low numbers of bacteria. J Biomed Mater Res 5:185–203
Klosterhalfen B, Klinge U, Hermanns B, Schumpelick V (2000) Pathology of traditional hernia nets for hernia repair after long-term implantation in humans. Chirurg 71:43–51.S
Greca FH, de Paula JB, Biondo-Simoes ML, da Costa FD, da Silva AP, Time S, Mansur A (2001) The influence of differing pore sizes on the biocompatibility of two polypropylene meshes in the repair of abdominal defects: experimental study in dogs. Hernia 5:59–64
Junge K, Klinge U, Prescher A, Giboni P, Niewiera M, Schumpelick V (2001) Elasticity of the anterior abdominal wall and impact for reparation of incisional hernias using mesh implants. Hernia 5:113–8
Klinge U, Junge K, Spellerburg B, Piroth C, Klosterhalfen B, Schumpelick V (2002) Do multifilament allopolastic meshes increase the infection rate? Analysis of the polymeric surface, the bacterial adherence and the in vivo consequences in a rat model. J Biomed Mater Res 63:765–71
Serbetci K, Kulacoglu H, Devay A, Hasirci N (2007) Effects of resterilization on mechanical properties of polypropylene meshes. Am J Surg 194:375–9
Clave A, Yahi H, Hammou J-C, Montanari S, Gounon P, Clave H (2010) Polypropylene as a reinforcement in pelvic surgery is not inert: comparative analysis of 100 explants. Internat Urogyn J 21:261–70
Conflicts of interest
Paid consultant, American Medical Systems; expert testimony in mesh litigation.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
A related article can be found at doi:10.1007/s00192-011-1405-4.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Ostergard, D.R. Degradation, infection and heat effects on polypropylene mesh for pelvic implantation: what was known and when it was known. Int Urogynecol J 22, 771–774 (2011). https://doi.org/10.1007/s00192-011-1399-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1399-y