Abstract
Having adopted a dynamic zero-COVID strategy to respond to SARS-CoV-2 variants with higher transmissibility since August 2021, China is now considering whether, and for how long, this policy can remain in place. The debate has thus shifted towards the identification of mitigation strategies for minimizing disruption to the healthcare system in the case of a nationwide epidemic. To this aim, we developed an age-structured stochastic compartmental susceptible-latent-infectious-removed-susceptible model of SARS-CoV-2 transmission calibrated on the initial growth phase for the 2022 Omicron outbreak in Shanghai, to project COVID-19 burden (that is, number of cases, patients requiring hospitalization and intensive care, and deaths) under hypothetical mitigation scenarios. The model also considers age-specific vaccine coverage data, vaccine efficacy against different clinical endpoints, waning of immunity, different antiviral therapies and nonpharmaceutical interventions. We find that the level of immunity induced by the March 2022 vaccination campaign would be insufficient to prevent an Omicron wave that would result in exceeding critical care capacity with a projected intensive care unit peak demand of 15.6 times the existing capacity and causing approximately 1.55 million deaths. However, we also estimate that protecting vulnerable individuals by ensuring accessibility to vaccines and antiviral therapies, and maintaining implementation of nonpharmaceutical interventions could be sufficient to prevent overwhelming the healthcare system, suggesting that these factors should be points of emphasis in future mitigation policies.
Similar content being viewed by others
Main
First discovered in Southern Africa in November 2021 (ref. 1), the Omicron variant of SARS-CoV-2 has spread swiftly across the world and replaced the Delta variant to become the dominant strain globally2. Omicron has demonstrated an increased transmissibility relative to Delta1,3,4,5 and immune escape capability6,7. Together with the progressive waning of the protection against the infection associated with previous infections and/or vaccination8,9,10,11,12, these characteristics have led to large Omicron epidemics in most countries13. Despite signs of a possibly lower clinical severity than Delta14,15,16,17,18, the sheer volume of Omicron infections has strained healthcare systems worldwide, including in the United States19,20 and the United Kingdom21. For instance, in the United Kingdom, the Omicron wave has led to higher infection rates than during the second wave in the winter of 2021, with substantial hospitalizations and deaths (over 1,000 deaths reported per week between 14 January and 4 February 2022)21.
After controlling the initial epidemic wave in Hubei in early 2020, China has deployed multilayer nonpharmaceutical intervention (NPI) protocols to contain sporadic COVID-19 outbreaks, largely introduced from international travelers. Maintaining a low infection rate in the general population throughout the pandemic has provided China time to mass immunize the population against SARS-CoV-2. As of 18 April 2022, 91.4% of the population aged ≥3 years has received the full primary schedule of the COVID-19 vaccination (either inactivated vaccines administered on a two-dose schedule, or recombinant subunit vaccines administered on a three-dose schedule or recombinant adenovirus type-5-vectored vaccines administered as a single dose); 53.7% of those vaccinated have received a booster shot22. However, vaccine-induced population immunity may be insufficient to prevent COVID-19 outbreaks. From 1 March to 22 April 2022, more than 500,000 local Omicron infections have been reported in almost all provinces across China, with most (about 93%) occurring in Shanghai22. To contain the highly infectious and immune evasive Omicron variant, additional NPI measures will be required to maintain the dynamic zero-COVID policy. This policy, adopted by China to respond to SARS-CoV-2 variants with higher transmissibility since August 2021, consists of a comprehensive set of measures to identify SARS-CoV-2 infections and stop any transmission chain, thus repeatedly zeroing local transmission23. Whether, and for how long, a zero-COVID policy can remain in place is questionable and, as recommended by the WHO24, every country should be prepared to chart its own path to transit from a pandemic to an endemic phase while accounting for local epidemiology, vaccination levels, population immunity and the strength of health systems. In this regard, as of May 2022, two approved antiviral treatments (BRII-196/BRII-198 combination and nirmatrelvir tablet/ritonavir tablet combination package) have been used in China, providing a new tool against COVID-19 (refs. 25,26).
Here, we explore the feasibility of a COVID-19 mitigation strategy to safeguard China’s shift from pandemic containment to mitigation, while minimizing the disease burden. Specifically, we leverage a mathematical model (Extended Data Fig. 1) to simulate a hypothetical Omicron wave in China based on data from the 2022 Omicron outbreak in Shanghai (Extended Data Fig. 2), project the demand for hospital beds and intensive care units (ICUs) and explore mitigation strategies combining vaccinations, antiviral therapies and NPIs to reduce COVID-19 burden while preventing the healthcare system being overwhelmed.
Results
Baseline scenario
The baseline scenario considers a homologous booster vaccination in the absence of strict NPIs and antiviral therapies. Specifically, the following conditions are simulated: (1) the introduction of 20 Omicron-infected individuals into the Chinese population on 1 March 2022; (2) the reproduction number (R) at the beginning of the simulation is set at 3.9 (when considering the partial protection of the population induced by vaccination, the reproduction number decreases to 3.4, in agreement with what we estimated for the early phase (from 1 March to 8 March 2022) of the epidemic in Shanghai (Extended Data Fig. 2), before strict control measures were implemented (Methods)); (3) booster doses of inactivated vaccines are rolled out at a speed of 5 million doses per day from 1 March 2022 (before that date the daily vaccination rates were informed by the cumulative number of doses administered in China); (4) 90% of individuals who have completed the primary vaccination schedule by at least 6 months receive a booster shot; (5) vaccine efficacy (VE) is set according to the values reported in Supplementary Table 1, considering a low immune escape scenario with same VEs against hospitalization and deaths between homologous booster and heterologous booster vaccination as observed in Hong Kong27 and (6) antiviral therapies are not distributed.
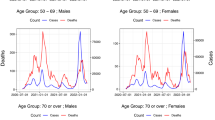
Our simulated baseline scenario suggests that, in the absence of strict NPIs, the introduction of the Omicron variant in China in March 2022 could have the potential to generate a tsunami of COVID-19 cases. Over a 6-month simulation period, such an epidemic is projected to cause 112.2 million symptomatic cases (79.58 per 1,000 individuals), 5.1 million hospital (non-ICU) admissions (3.60 per 1,000 individuals), 2.7 million ICU admissions (1.89 per 1,000 individuals) and 1.6 million deaths (1.10 per 1,000 individuals), with a main wave occurring between May and July 2022 (Figs. 1 and 2).
a, Daily hospital (non-ICU) admissions per 10,000 individuals. b, Epidemiological status of hospitalized (non-ICU) patients. c, Age distribution of hospitalized (non-ICU) patients. d, Distribution of hospitalized (non-ICU) patients per 10,000 by age group and epidemiological status. e, Daily ICU admissions per 10,000 individuals. f, Epidemiological status of ICU patients. g, Age distribution of ICU patients. h, Distribution of ICU patients per 10,000 by age group and epidemiological status. i, Daily deaths per 10,000 individuals. j, Epidemiological status of deaths. k, Age distribution of deaths. l, Distribution of deaths per 10,000 by age group and epidemiological status. In panels b, f and j, susceptible refers to individuals who do not receive COVID-19 vaccines; primary refers to those individuals who have received at least one dose of COVID-19 vaccine, considering a primary vaccination which entails a two-dose schedule; booster refers to those individuals who have received a third dose; recovery refers to individuals who have recovered from SARS-CoV-2 Omicron infection. Data are presented as median with 2.5% and 97.5% quantiles of n = 200 simulations.
According to our model simulations, 41.3% of non-ICU hospitalizations and 28.2% of ICU admissions would occur among vaccinated individuals. Most non-ICU hospitalizations are estimated to occur in the adult population (26.6% among individuals aged 18–59 years and 59.1% among individuals aged ≥60 years), while over 90% of ICU admissions would occur among individuals aged ≥60 years (Fig. 1). Most deaths (76.7%) are estimated to occur among nonvaccinated individuals, despite representing only 12.1% of the population (Fig. 1). Unvaccinated individuals aged ≥60 years are projected to account for 74.7% of the total number of deaths due to the gap in vaccination coverage in this portion of the population; approximately 52 million people aged ≥60 years are not fully vaccinated as of 17 March 2022 (ref. 28).
In addition to presenting analyses for a national average, we analyze three highly diverse areas of China: Shanghai, Shandong and Shanxi. For each of these areas, we consider a specific vaccination coverage, age structure of the population, contact patterns of the population (Supplementary Fig. 1) and number of available hospital beds and ICUs (Supplementary Table 2). The results show a considerable heterogeneity across the different areas. For example, the number of deaths per 1,000 inhabitants in the baseline scenario is projected to be 1.79 in Shanghai (where, as of 15 April 2022, 62% of individuals aged ≥60 years were fully vaccinated and 38% had received a booster dose29) compared with 0.84 in Shandong (the province with the highest vaccination coverage in individuals aged ≥60 years among the four settings; as of 21 March 2022, 89.16% of this population were fully vaccinated and 72.45% had received a booster dose30) (Fig. 2).
To evaluate the impact of an uncontrolled Omicron epidemic on the national healthcare system, we considered that all COVID-19 hospitalizations require hospital beds for respiratory illness and that critically ill cases require ICU beds, and computed the corresponding demands. At the national scale, it is estimated that 1.57 million hospital beds for respiratory illness would be required at the epidemic peak, which is fewer than the number of existing hospital beds for respiratory illness (3.1 million) in China31. However, the peak demand of ICU beds (1.00 million) corresponds to 15.6 times the number of existing ICU beds in China (that is, 64,000)31. The period of ICU bed shortage is estimated to last for approximately 44 days (Fig. 3). In the regional analyses, substantial shortages of ICU beds were also predicted to occur in Shanghai, Shandong and Shanxi province (Extended Data Fig. 3).
a, Daily demand of hospital (non-ICU) beds. b, Daily demand of ICU beds. In b, the green dashed line indicates the number of ICU beds available in China, and the inset plot shows days of shortage of ICU beds as a function of the number of insufficient ICU beds compared with the capacity of ICU beds. The curves in the inset are smoothed by B-spline with 8 d.f. The scenarios included in legend are as follows: subunit vaccines refer to using a third dose of subunit vaccines as booster after two doses of inactivated vaccines as priming. Vaccinating elderly refers to vaccinating approximately 52 million people aged ≥60 years who have not yet been vaccinated as of 17 March 2022. 50% uptake and 80% efficacy corresponds to a scenario where 50% of symptomatic cases receive an antiviral therapy with an efficacy of 80% in preventing hospitalization and death. 100% uptake and 89% efficacy corresponds to a scenario where all symptomatic cases receive an antiviral therapy with an efficacy of 89% in preventing hospitalization and death. School and workplace closure corresponds to a scenario where, on the top of baseline strategy, all schools and workplaces remain closed for the duration of the epidemic. Rt: 3.0 and 2.0 correspond to scenarios assuming different levels of NPIs leading to reduced values of the reproduction number. Note that no strict NPI is implemented in the baseline scenario. Data are presented as median with 2.5% and 97.5% quantiles of n = 200 simulations.
When considering a more conservative scenario on the immune escape of the Omicron variant (referred as to high immune escape scenario), with (1) lower VEs against all clinical endpoints as compared with low immune escape scenario, and (2) lower VEs against hospitalization and deaths for homologous booster as compared with heterologous booster vaccination (as observed in Brazil32, Supplementary Table 1), the projected number of hospitalizations, ICU admissions and deaths at the national level would increase by 77.3%, 62.1% and 50.2%, respectively (Extended Data Fig. 4).
Impact of individual mitigation strategies
We investigated separately the impact of three categories of strategies to mitigate COVID-19 burden: (1) vaccination, including heterologous booster doses and promoting vaccination coverage among unvaccinated individuals aged ≥60 years, (2) antiviral therapies and (3) NPIs. Regarding booster vaccination, if we consider the administration of a heterologous booster based on a subunit vaccine (subunit vaccines scenario) in the low immune escape scenario, little difference would be observed in terms of COVID-19 burden (Fig. 4); on the other hand, in the high immune escape scenario, a larger decrease of COVID-19 burden (8.4% in the number of deaths and 17.7% in the number of hospital admissions) could be achieved by administrating a heterologous booster based on a subunit vaccine (Extended Data Fig. 5). Filling the gap in the vaccination coverage among the elderly (that is, vaccinating all eligible individuals aged 60 years or more), including both primary and booster vaccination as in the baseline scenario (vaccinating elderly scenario) would lead to a 33.8%, 54.1% and 60.8% decrease in hospital admissions, ICU admissions and deaths, respectively (Fig. 4).
a, Cumulative number of hospital (non-ICU) admissions. b, Cumulative number of ICU admissions. c, Cumulative number of deaths. The scenarios indicated on the y axis are as follows: subunit vaccines refer to using a third dose of subunit vaccines as booster after two doses of inactivated vaccines as priming. Vaccinating elderly refers to vaccinating approximately 52 million people aged ≥60 years have not been vaccinated yet as of 17 March 2022. 50% uptake and 80% efficacy corresponds to a scenario where 50% of symptomatic cases receive an antiviral therapy with an efficacy of 80% in preventing hospitalization and death. 100% uptake and 89% efficacy corresponds to a scenario where all symptomatic cases receive an antiviral therapy with an efficacy of 89% in preventing hospitalization and death. School closure corresponds to a scenario where, on the top of baseline strategy, all schools remain closed for the duration of the epidemic. Similarly, school and workplace closure corresponds to a scenario, where on the top of baseline strategy, all schools and workplaces remain closed for the duration of the epidemic. Rt: 3.0, 2.5 and 2.0 correspond to scenarios assuming different levels of NPIs leading to reduced values of the reproduction number. Note that no strict NPI is implemented in the baseline scenario. Data are presented as median with 2.5% and 97.5% quantiles of n = 200 simulations.
In the absence of NPIs, assuming that 50% of symptomatic cases could be treated with the approved Chinese COVID-19 BRII-196/BRII-198 combination therapy, which has been reported to be 80% effective in preventing hospitalization and death33, a 36.5%, 39.9% and 40.0% decrease in hospital admissions, ICU admissions and deaths is estimated (50% uptake and 80% efficacy scenario). In the best-case scenario in which all symptomatic cases are treated with the highly efficacious oral COVID-19 drug nirmatrelvir tablet/ritonavir tablet combination (which is 89% effective in preventing hospitalization and death34 and has already been used in China26), the number of hospital admissions, ICU admissions and deaths could be reduced substantially by 81.2%, 88.8% and 88.9% (100% uptake and 89% efficacy scenario) (Fig. 4).
We then modeled the impact of introducing different levels of NPIs (in the presence of vaccination, but absence of antiviral therapies). First, we tested the implementation of a national-level school closure strategy (school closure scenario); although the number of infections decrease by 3.5%, COVID-19 burden does not, due to a shift in the age distribution of infections towards older ages. Additionally, closing all workplaces (school and workplace closure scenario) would lead to a decrease of 23.8%, 13.1% and 22.4% for the number of hospitalizations, ICU admissions and deaths, respectively. Second, we considered a scenario where NPIs equally reduce the risk of infection across all age groups, and we simulated different intensity of NPIs leading to Rt ≤ 3 (similar to values observed in England35 and India36 during the Omicron wave in winter 2021–2022). In this scenario, only the adoption of NPIs capable of reducing Rt to values ≤2 would lead to a substantial decrease in health outcomes (namely, a decrease of 40.1%, 33.4% and 48.6% of the number of hospitalizations, ICU admissions and deaths, respectively) (Fig. 4).
In summary, none of the scenarios analyzed is estimated to have the potential to reduce the number of COVID-19 deaths to a level closer to the annual influenza-related excess deaths in China (88,000)37 (Fig. 4). In all scenarios, the peak demand for ICUs is projected to be 1.7–14.8 times the maximum capacity, with a total of 19–48 days of bed shortages (Fig. 3b). We emphasize that closing all schools and workplaces as well as implementing stringent NPIs to reduce Rt to 2 would result in highly delayed epidemics that extend beyond our projection window (6 months); as such, their final impact is not evaluated in this analysis (Fig. 3b).
Impact of combined mitigation strategies
None of the investigated individual mitigation strategies alone is capable of reducing the death toll to the level of an influenza season or to prevent exceeding critical care capacity (Figs. 3 and 4). Here, we assessed the effects of synergetic strategies leveraging heterologous booster vaccination, increasing vaccination coverage among the unvaccinated individuals aged 60 years or more, distributions of antiviral therapies and adoption of NPIs at the same time (Fig. 5).
a, Peak hospital (non-ICU) bed occupancy, with red numbers indicating where peak hospital bed demand is lower than the bed capacity for respiratory illness in China. b, Peak ICU bed occupancy, with red numbers indicating where peak ICU bed demand is below the existing ICU capacity in China. c, Cumulative death tolls, with red numbers indicating where the number of deaths is below the annual influenza-related excess death toll in China (that is, 88,000 deaths37). The circular-Manhattan plot from the innermost concentric circle to the outermost concentric circle indicates the combinations of adopting different intervention measures: homologous (inactivated) or heterologous (subunit) booster regimen; whether the approximately 52 million people aged ≥60 years who have not been vaccinated yet as of 17 March 2022 are vaccinated or not; receiving antiviral therapies with an efficacy of 80% or 89% in preventing hospitalization and death; 50% or 100% symptomatic cases receiving an antiviral therapy; Rt representing varying intensity of NPIs. Rt = 3.9 corresponds to the scenario in the absence of strict NPIs. Data are presented as median of n = 200 simulations.
None of the simulated interventions is projected to exceed the national capacity of hospital bed capacity for respiratory illness. Instead, a synergetic effort of combining different strategies would be needed to prevent exceeding ICU capacity and limiting the number of deaths to a value comparable to that of seasonal influenza. According to our analysis, key aspects of this synergetic effort are the increase of vaccine uptake in the elderly and the widespread use of antiviral therapies (Fig. 5). If these two conditions are not met, relying on NPIs capable of reducing R to ≤2 is needed to prevent overwhelming the healthcare system.
Discussion
Using a stochastic dynamic model of SARS-CoV-2 transmission, our study projects the COVID-19 burden caused by the importation of Omicron infections in mainland China, should the dynamic zero-COVID policy be lifted. In the context of the vaccination strategy adopted until March 2022, we estimated that the introduction of the Omicron variant would cause substantial surges in hospitalizations, ICU admissions and deaths, and would overwhelm the healthcare system with an estimated burden of 15.6 times the available ICU capacity.
Should an Omicron variant epidemic be allowed to spread uncontrolled in mainland China, we project 1.10 deaths per 1,000 inhabitants over a 6-month period. By comparison, 187,372 deaths have been reported in the United States38 (that is, 0.57 deaths per 1,000 inhabitants) over the period from 15 December 2021 to 15 April 2022, roughly corresponding to the Omicron wave. We estimate that around 77% of the death toll in China would occur in unvaccinated individuals, with most deaths occurring among unvaccinated individuals aged 60 years or more (52 million people). A similar trend has been observed in the Omicron-driven fifth COVID-19 wave in Hong Kong Special Administrative Region (SAR) of China, which began in early 2022 (ref. 39). Our findings highlight the key role of increasing vaccine uptake rate among the elderly to limit COVID-19 burden and to prevent overwhelming the healthcare system. A second key factor to reach these goals is represented by the widespread and timely distribution of a highly efficacious antiviral therapy. When both vaccine uptake in the elderly is substantially increased (97%) and 50% or more of symptomatic infections are treated with antiviral therapies, the peak occupancy of ICUs may not exceed the national capacity and the death toll may be comparable to that of seasonal influenza. In the absence of these two conditions, the most optimistic strategy to prevent overwhelming of the healthcare system seems to be reliance on strict NPIs.
China is a highly diverse country with urban megalopolises on the eastern seaboard and rural areas in the northwest. Such diversity is also reflected by heterogeneous vaccination coverage, demographic structure of the population, mixing patterns and capacity of the healthcare system. When accounting for these heterogeneities, our simulations show considerable differences in the projected COVID-19 burden for different areas of China. According to our projections, the population of Shanghai would experience a COVID-19 burden higher than that of other areas such as Shandong and Shanxi. This increased burden would be led by a much larger incidence of severe infections in the population aged 60 years or older, which is associated with a lower vaccination coverage in this segment of the population. This result confirms the importance of filling the vaccination gap among the elderly and the need to tailor interventions to the specific immunological landscape of the population.
Our study has several limitations. First, we assumed that the mortality rate remains constant over the projection period; however, studies have suggested that the mortality rate may increase during periods of high strain on hospital services40,41. Second, although we conducted a comprehensive literature search, the epidemiological characteristics of Omicron, clinical severity, VEs of primary and booster vaccination and its persistence against different clinical endpoints, as well as the effectiveness of antiviral therapies, are not fully understood. For this reason, we have conducted extensive sensitivity analyses to explore the impact of the uncertainty of model parameters. Third, data on antiviral therapy availability by region are unknown and thus not included in our analysis. Possible regional differences in stockpiles of antiviral therapies could widen the already large differences in COVID-19 burden that we have estimated among the study locations.
In conclusion, should the Omicron outbreak continue unabated, despite a primary vaccination coverage of ≥90% and homologous booster vaccination coverage of ≥40% as of March 2022, we project that the Chinese healthcare system will be overwhelmed with a considerable shortage of ICUs. The contemporary increasing of vaccine uptake in the elderly and widespread distribution of antiviral therapies or the implementation of strict NPIs would be needed to prevent overwhelming of the healthcare system and to reduce the death toll of an epidemic wave to a level comparable with that of an influenza season. Protecting vulnerable individuals by ensuring access to vaccination and antiviral therapies, as well as maintaining implementation of NPIs (for example, mask-wearing, enhanced testing, social distancing and reducing mass gatherings), should be emphasized, together with tailoring region-specific interventions. In the long term, improving ventilation, strengthening critical care capacity and the development of new highly efficacious vaccines with long-term immune persistence would be key priorities.
Methods
This modeling study relies on publicly available aggregated data only. As such, institutional review and informed consent are waived by the Institutional Review Board of the School of Public Health, Fudan University (Shanghai, China).
Model SARS-CoV-2 transmission and vaccination
We developed an age-structured stochastic compartmental susceptible-latent-infectious-removed-susceptible model (Extended Data Fig. 1) to simulate the transmission of the SARS-CoV-2 Omicron variant in China. The model considers 14 age groups (0–2, 3–11, 12–17, 18–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69 and ≥70 years) and age-mixing patterns for China before the COVID-19 pandemic42. The model accounts for primary and booster vaccination, disease progression, antiviral therapies and waning immunity. All compartments and parameters are defined in Supplementary Tables 3 and 4. Transitions between compartments are simulated through a stochastic chain binomial process43. For instance, susceptible individuals move to the latent compartment at the rate \(\Delta _\mathrm{a}(t)\sim \mathrm{Binomial}\left( {S_\mathrm{a}(t),1 - {\mathrm{e}}^{ - \lambda _\mathrm{a}\left( t \right)}} \right)\), where λa(t) is the force of infection for age group a at time t.
Baseline simulations were seeded with 20 imported infections on 1 March 2022 and run forward for 6 months. We consider five and ten seeds as sensitivity analyses (Supplementary Fig. 2). Upon infection with SARS-CoV-2, susceptible individuals (S) enter an exposed (latent) compartment (L) before becoming infectious. We consider that children and adolescents were less susceptible to infection compared with adults44,45. A sensitivity analysis considering homogeneous susceptibility across age groups is presented in Supplementary Fig. 3. Exposed individuals stay in their compartment for an average of 1/γE = 1.2 days before moving to either asymptomatic (IA) or symptomatic (IS) compartments according to the age-specific probability of being asymptomatic (\(1 - P_a^s\)). No difference in infectiousness between asymptomatic and symptomatic individuals was considered in the main analyses46, whereas asymptomatic individuals were considered to be 65% less infectious than symptomatic ones in a sensitivity analysis47 (Supplementary Fig. 4). An age-dependent proportion (\(P_a^h\)) of symptomatic cases require hospitalization (H), while the rest of symptomatic cases and all asymptomatic infections recover naturally (R) (Extended Data Fig. 1a). We assume asymptomatic infections and nonhospitalized symptomatic cases to stay in their compartments for an average of 1/γI = 5.6 days, thus resulting in mean intrinsic generation time of 6.8 days, as previously estimated for Omicron48 (Supplementary Table 5).
For patients requiring hospitalization (H), the average time from symptom onset to hospital admission was 1/γSH = 2.2 days (ref. 49). We assume that hospitalized patients do not transmit the virus. We divided the hospital settings (H) into two parts: the general ward (Hosp) and ICU ward (ICU), as illustrated in Extended Data Fig. 1b. Once admitted to hospital, a patient either remains in the general ward until discharge or is transferred to an ICU according to an age-dependent ICU admission risk. We assume that patients admitted to an ICU entered the ICU on the same day they were admitted to hospital. Patients in the general ward (or ICU) could either stay in the general ward (or ICU) until they are discharged or die, based on the corresponding mortality risk. We assume that all deaths occur among hospitalized patients.
To capture the potential impact of newly available antiviral therapies, we divided symptomatic cases (IS) into two categories: those who timely received an antiviral therapy after symptom onset, and those who did not (Extended Data Fig. 1c).
All compartments and transition flows are duplicated into parallel branches that represent primary (V) and booster (B) vaccinations (Extended Data Fig. 1d). We assume that only susceptible individuals in compartment S are eligible for primary vaccination. To describe the recommended two-dose primary vaccination (common to the two inactivated vaccines currently widely used in China: Sinovac/CoronaVac and Sinopharm/BBIBP-CorV), compartment V was further stratified into two vaccination strata (V1 and V2), differentiating individuals who have received one or two doses, respectively. Only uninfected individuals who have completed their primary vaccination schedules by 6 months (1/ωP) will receive a booster shot (B). Each dose produces a vaccine protection (V1e, V2e, Be) after an average of 14 days (1/ω1, 1/ω3 and 1/ω4).
We model VE against infection using a ‘leaky’ vaccine in which all vaccinated individuals are exposed to a lower risk of infection, which is 1 – VE times that of nonvaccinated individuals50. Like vaccination-induced protection, infection-induced immunity wanes over time (Extended Data Fig. 1d). After an average of 180 days (1/ωP) since the second dose, primary-vaccinated individuals move to a new compartment (‘waned vaccine effectiveness’, V2W); individuals in this compartment are ready for receiving their booster shots. Likewise, 180 days (1/ωB) after the booster shot, boosted individuals move to a new compartment (‘waned vaccine effectiveness’, BW). Waning of infection-induced immunity acts in a manner different from that of the vaccine. Individuals who have recovered from SARS-CoV-2 infection (R) are protected against reinfection with the same variant for an exponentially distributed duration with mean 1/ωR days, after which they move back to the susceptible compartment. The transition rates for vaccine- and infection-induced immunity processes are defined in Supplementary Table 6 (ref. 51). The VEs against different clinical endpoints in the different stages of vaccine protection are reported in Supplementary Table 1. Details are reported in Vaccine effectiveness.
Model of COVID-19 burden
Age-specific risks
To measure the burden (that is, hospitalizations, ICU admissions and deaths) and the strain of the healthcare system, we rely on the age-specific infection fatality risk (IFR) and infection hospitalization risk among unvaccinated individuals from the Omicron wave in Hong Kong SAR, China39. The Hong Kong Center for Health Protection publishes reported case fatality ratios by age group and vaccination status52, and compares the age profiles of reported cases against resident population53. Since the age profile of cumulative reported cases is very similar to the resident population by the end of 2021 in Hong Kong SAR, we assume the undetected infections have the same age profile as the reported cases. We thus estimate the age-specific IFR by dividing the age-specific case fatality ratios among unvaccinated individuals by the overall infection-reporting ratio. A modeling report on the fifth wave of COVID-19 in Hong Kong SAR54 estimates that around 4.5 million residents of Hong Kong had been infected by 21 April 2022, as of which day 1.18 million cumulative case were reported. We further calculate age-specific infection hospitalization risk from the Hong Kong Omicron wave39 by dividing the estimated IFR by the age-specific fatality risk among hospitalized patients who were not fully vaccinated (B. J. Cowling, personal communication, 2022) (Supplementary Table 7).
For the age-specific ICU admission risk of hospitalized patients, we adjusted the ICU admission risk associated with the ancestral lineage reported in China55, by the ratio of the overall ICU admission risk among unvaccinated hospitalized patients infected with the Omicron variant (19.0% (ref. 56)) and those infected with the ancestral lineage (6.4% (ref. 55)). The estimated age-specific risks of disease progression are presented in Supplementary Tables 7 and 8 (ref. 57).
Duration of hospital and ICU stay
We set the length of stay in hospital to 6 days; 8 days are considered for non-ICU hospitalizations with fatal outcomes based on observations in the Hong Kong Omicron wave39 (B. J. Cowling, personal communication, 2022). We assumed the ICU length of stay to be 8 days, consistent with literature reports58,59.
Healthcare resources
As of 2020, a total of 9.1 million hospital beds were available in China. Among them, 3.14 million were reserved for respiratory illness (including hospital beds in departments of internal medicine, pediatrics, infectious disease and ICUs), 64,000 of which are ICUs31.
Model validation against the Omicron outbreak in Shanghai
We calibrated the transmissibility and proportion of symptomatic cases to the field data of the Omicron BA.2 variant outbreak in Shanghai, China. We used a Bayesian approach60 to estimate the net reproduction number Rt for the initial phase (from 1 March to 8 March 2022) of the epidemic in Shanghai, before strict control measures were implemented. The method is based on the analysis of the epidemic curve of symptomatic cases and on the knowledge of the generation time, which is assumed to be Gamma distributed with mean 6.8 days (shape = 2.39, scale = 2.95) as estimated for the Omicron variant in a previous study48. The resulting estimate of the average reproduction number Rt is 3.4. We then follow the approach in Marziano et al.61 based on the next generation matrix to calculate the model transmission rate from the estimated reproduction number while accounting for the vaccine-induced partial protection of the population. When removing the effect of vaccination, we estimated the reproduction number R of the Omicron BA.2 variant to be 3.9 at the beginning of the 2022 outbreak in Shanghai. Such an estimate is conditional on the situation on the ground at the beginning of March 2022, where, although no strict NPIs were implemented, a mask mandate was still in place and the behavior of the population may have been different from prepandemic standards.
City-wide screenings are being conducted frequently throughout the course of the Shanghai outbreak allowing the identification of most infected individuals, regardless of the presence/absence of symptoms. Therefore, to estimate the association between symptoms and infection, we simulated our compartmental model for the population of Shanghai (which also considers city-specific vaccination rates) assuming Rt to be 3.4. We then modulated the age-specific probability of developing symptoms62 by a scaling factor that is chosen to fit both the curves of symptomatic and asymptomatic infections in Shanghai between 1 March and 8 April 2022 (Extended Data Fig. 2). We further adjusted the calibrated age-specific probability of developing symptoms by the ratio of the proportion of confirmed cases among total infections observed in Shanghai during the initial phase (from 1 March to 8 April 2022) (3.50%) to that from 1 March to 28 April 2022 (9.24%)63.
Finally, as a sensitivity analysis, we also calibrated the model using a shorter generation time, in line with estimates for the Delta variant in the United Kingdom (4.7 days; ref. 64) (Supplementary Fig. 5).
Mitigation with vaccination
A mass vaccination campaign has been launched in China since December 2020 (ref. 65). On 3 October 2021, a homologous booster vaccination campaign (relying on the same vaccine as the initial inactivated vaccine shots) has been initiated among individuals aged ≥18 years who completed primary vaccination at least 6 months earlier66,67. As of 12 April 2022, >90% of populations aged ≥3 years have completed primary vaccination and >50% of the populations has received a booster dose68. Compared with other age groups (86.4%, 100% and 92.3% fully vaccinated individuals for the age groups 3–11, 12–17 and 18–59 years, respectively), individuals aged ≥60 years have the lowest vaccination coverage (about 80%)69, corresponding to approximately 52 million unvaccinated individuals28.
From 1 March 2022 onwards, homologous booster rollout was set at 5 million doses per day in the baseline analysis. Sensitivity analyses on heterologous booster vaccination using subunit, mRNA, and vector vaccines were conducted (Supplementary Fig. 6). The only difference between heterologous and homologous booster considered in the model is VE (values reported in Supplementary Table 1). Vaccine coverage over time and by age group for the baseline scenario is presented in Supplementary Fig. 7.
Vaccine effectiveness
We considered different VEs against different clinical endpoints (namely, infection, symptomatic illness, hospitalization and death) and onward transmission. As shown in Supplementary Table 1, VEs against these clinical outcomes at the following five time points are considered: 14 days after receiving the first dose, 14 days after receiving the second dose, 14 days after the booster dose, 6 months after the second dose of primary 2-dose vaccination (2W) and 6 months after the booster dose (BW). To account for the decay of VEs, either 6 months after the second dose of primary vaccination or after the booster dose, vaccinated individuals move to the ‘waned vaccine effectiveness’ compartments V2W and BW, respectively.
VEs against symptomatic disease, hospitalization and death after receiving two doses of inactivated vaccines, a homologous booster using inactivated vaccines and a heterologous booster using mRNA vaccines were estimated during the Omicron waves in Hong Kong or Brazil27,32. For other VEs without field estimates, we used a verified statistical model70 to predict vaccine protection based on the levels of neutralizing antibody titers (NATs) against Omicron between different booster regimens and time points summarized in Supplementary Table 9 (refs. 71,72,73,74). The Omicron variant shows very high immune escape potential. Peiris et al.75 found a 6.4-fold and 9.7-fold decrease in the level of NATs against Omicron 6 months after administering two doses and 1 month after administering a booster dose of inactivated vaccines, respectively, compared with those against the ancestral lineage (low immune escape scenario). We further conducted a sensitivity analysis for a high immune escape scenario, which considers a 19.1-fold decrease in the NAT against Omicron both after administering two doses and a booster dose of inactivated vaccines, compared with that against the ancestral lineage76. For VEs against symptomatic illness, hospitalization, and death, we use conditional VEs, which are calculated according to the formulas presented in Supplementary Table 10.
Mitigation through antiviral therapies
A homegrown monoclonal neutralizing antibody therapy (BRII-196/BRII-198 combination) and an imported antiviral therapy (nirmatrelvir tablet/ritonavir tablet combination) have been approved for emergency use in China25,26. In the baseline scenario, we do not consider antiviral therapies. To quantify the mitigating effect of antiviral therapies, we simulated two alternative scenarios: (1) 50% of symptomatic cases will receive an antiviral therapy with an efficacy of 80% in preventing hospitalizations and deaths (in agreement with the estimate for the Chinese manufactured BRII-196/BRII-198 combination)33, and (2) 100% of symptomatic cases will receive an antiviral therapy with an efficacy of 89% in preventing hospitalizations and deaths (in agreement with the estimate for the imported nirmatrelvir tablet/ritonavir tablet combination34,77). Only symptomatic cases of patients aged ≥12 years are eligible to receive COVID-19 antiviral therapies25 (Supplementary Table 6). The rationale for the 50% treatment uptake scenario is that not all symptomatic cases may be promptly identified, thus leading either to receive the treatment well after symptom onset (and thus the effectiveness of the antiviral therapy is reduced) or to entirely missing potential eligible individuals. The 100% treatment uptake scenario represents an ideal scenario where all eligible symptomatic infections receive the treatment at the peak of its efficacy.
Mitigation through NPIs
We tested the impact of NPIs in two ways: (1) implementing a national school closure or a national school and workplace closure by removing contacts that occurred in schools or workplaces from the baseline mixing patterns (Supplementary Fig. 1) and (2) reducing effective contacts equally across age groups, which is modeled as a reduction in the reproduction number; specifically, we considered Rt = 2.0, 2.5, 3.0 and 3.9 that represent varying intensities of NPIs (Supplementary Table 5).
Geographical heterogeneity across the Chinese population
To account for within-China heterogeneity, we run the baseline analysis for three other highly diverse contexts: (1) an urbanized setting with a relatively low vaccine coverage (Shanghai), (2) a rural setting with a relatively low vaccine coverage (Shanxi, a central province in China) and (3) a high vaccination setting (Shandong, an eastern coastal province). In our analysis, these settings differ in terms of primary and booster vaccination coverages, age structure of the population, contact patterns of the population42, number of available hospital beds and ICUs31 (Supplementary Table 2 and Supplementary Fig. 1). The overall and age-specific incidence rates of different clinical endpoints over a 6-month simulated period across the three settings are compared with the ‘national average’.
Statistical analysis
For each scenario, we performed 200 stochastic simulations. The outcomes of these simulations determined the distribution of the number of symptomatic infections, hospital admissions, ICU admissions and deaths by age. We defined 95% credible intervals as quantiles 0.025 and 0.975 of the estimated distributions.
Reporting summary
Further information on research design is available in the Nature Research Reporting summary linked to this article.
Data availability
The data used in the study are provided in Supplementary Information and are available with the code on GitHub at https://github.com/DXW-sola1015/Model_Omicron_China.
Code availability
The codes used in this study are available on GitHub at https://github.com/DXW-sola1015/Model_Omicron_China.
References
Viana, R. Rapid epidemic expansion of the SARS-CoV-2 Omicron variant in southern Africa. Nature 603, 679–686 (2022).
Tracking of VOC Omicron. Global Initiative of Sharing All Influenza Data (GISAID) (29 January 2022); https://www.gisaid.org/hcov19-variants/
Lyngse, F.P. SARS-CoV-2 Omicron VOC transmission in Danish households. Preprint at medRXiv https://doi.org/10.1101/2021.12.27.21268278 (2021).
Pearson, C.A.B. et al. Bounding the levels of transmissibility & immune evasion of the Omicron variant in South Africa. Preprint at medRxiv https://doi.org/10.1101/2021.12.19.21268038 (2021).
Gozzi, N. et al. Preliminary modeling estimates of the relative transmissibility and immune escape of the Omicron SARS-CoV-2 variant of concern in South Africa. Preprint at medRxiv https://doi.org/10.1101/2022.01.04.22268721 (2022).
Lu, L. et al. Neutralization of SARS-CoV-2 Omicron variant by sera from BNT162b2 or Coronavac vaccine recipients. Clin. Infect. Dis. ciab1041 (2021).
Zhang, L. et al. The significant immune escape of pseudotyped SARS-CoV-2 variant omicron. Emerg. Microbes Infect. 11, 1–5 (2022).
Collier, A.-R. Y. et al. Differential kinetics of immune responses elicited by covid-19 vaccines. N. Engl. J. Med. 385, 2010–2012 (2021).
Levin, E. G. et al. Waning immune humoral response to BNT162b2 covid-19 vaccine over 6 months. N. Engl. J. Med. 385, e84 (2021).
Xin, Q. et al. Six-month follow-up of a booster dose of coronavac: two single-centre, double-blind, randomised, placebo-controlled phase 2 clinical trials. Preprint at SSRN https://doi.org/10.2139/ssrn.3991627 (2021).
Dan Jennifer, M. et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science 371, eabf4063 (2021).
Wheatley, A. K. et al. Evolution of immune responses to SARS-CoV-2 in mild-moderate COVID-19. Nat. Commun. 12, 1162 (2021).
WHO Coronavirus (COVID-19) Dashboard. World Health Organization (5 March 2022); https://covid19.who.int/
Wolter, N. et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study. Lancet 399, 437–446 (2022).
Maslo, C. et al. Characteristics and outcomes of hospitalized patients in South Africa during the COVID-19 Omicron wave compared with previous waves. JAMA 327, 583–584 (2022).
SARS-CoV-2 variants of concern and variants under investigation in England, Technical briefing: update on hospitalisation and vaccine effectiveness for Omicron VOC-21NOV-01 (B.1.1.529). UK Health Security Agency https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1044481/Technical-Briefing-31-Dec-2021-Omicron_severity_update.pdf (2021).
Wang, L. et al. Incidence Rates and Clinical Outcomes of SARS-CoV-2 Infection With the Omicron and Delta Variants in Children Younger Than 5 Years in the US. JAMA Pediatr. e220945 (2022).
Lewnard, J. A. et al. Clinical outcomes among patients infected with Omicron (B.1.1.529) SARS-CoV-2 variant in southern California. Preprint at medRxiv https://doi.org/10.1101/2022.01.11.22269045 (2022).
Iuliano, A. D. et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods—United States, December 2020–January 2022. MMWR Morb. Mortal. Wkly Rep. 71, 146–152 (2022).
Marks, K. J. et al. Hospitalizations of children and adolescents with laboratory-confirmed COVID-19—COVID-NET, 14 States, July 2021–January 2022. MMWR Morb. Mortal. Wkly Rep. 71, 271–278 (2022).
Coronavirus (COVID-19) latest insights. UK Office for National Statistics . https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19/latestinsights (2022).
Press conference held on situation regarding strict prevention and control of COVID-19 epidemic. The State Council Information Office, P.R.C. (19 April 2022); http://www.gov.cn/xinwen/gwylflkjz193/index.htm
Liu, J., Liu, M. & Liang, W. The dynamic COVID-zero strategy in China. China CDC Wkly. 4, 74–75 (2022).
COVID-19 Virtual Press conference transcript. World Health Organization (1 February 2022); https://www.who.int/publications/m/item/covid-19-virtual-press-conference-transcript-1-february-2022
Emergency approval of Brii Biosciences’ COVID-19 neutralizing antibody combination therapy: amubarvimab/romlusevimab combination (BRII-196/BRII-198) therapy. The National Medical Products Administration (NMPA) of China https://www.nmpa.gov.cn/yaowen/ypjgyw/20211208212528103.html (2021).
Emergency conditional approval of Pfizer’s COVID-19 therapy: nirmatrelvir tablet/ritonavir tablet combination package (i.e., Paxlovid) importation registration. The National Medical Products Administration (NMPA) of China https://www.nmpa.gov.cn/yaowen/ypjgyw/20220212085753142.html (2022).
McMenamin, M. E. et al. Vaccine effectiveness of two and three doses of BNT162b2 and CoronaVac against COVID-19 in Hong Kong. Preprint at medRxiv https://doi.org/10.1101/2022.03.22.22272769 (2022).
Press conference held on situation regarding strict prevention and control of COVID-19 epidemic. The State Council Information Office, P.R.C. (19 March 2022); http://www.gov.cn/xinwen/gwylflkjz187/index.htm
Press conference held on situation regarding prevetion and control of COVID-19 epidemic in Shanghai. Shanghai Municipal Health Commission (17 April 2022); https://j.eastday.com/p/1650166645036759
Press conference held on situation regarding prevetion and control of COVID-19 epidemic in Shandong province. People’s Government of Shandong Province (22 March 2022); http://www.shandong.gov.cn/vipchat1//home/site/82/3788/article.html
National Health Commission of China. China Health Statistics Yearbook 2021 (China Union Medical College Press, 2021).
Ranzani, O. T. et al. Effectiveness of an inactivated Covid-19 vaccine with homologous and heterologous boosters against the Omicron (B.1.1.529) variant. Preprint at medRxiv https://doi.org/10.1101/2022.03.30.22273193 (2022).
Brii Bio announces Amubarvimab/Romlusevimab combination received approval from NMPA as first COVID-19 neutralizing antibody combination therapy in China. Brii Biosciences (9 December 2021); https://www.briibio.com/news-detial.php?id=505
Hammond, J. et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19. N. Engl. J. Med. 386, 1397–1408 (2022).
Barnard, R. C., Davies, N. G., Pearson, C. A. B., Jit, M. & Edmunds, W. J. Projected epidemiological consequences of the Omicron SARS-CoV-2 variant in England, December 2021 to April 2022. Preprint at medRxiv https://doi.org/10.1101/2021.12.15.21267858 (2021).
Ranjan, R. Omicron impact in India: analysis of the ongoing COVID-19 third wave based on global data. Preprint at medRxiv https://doi.org/10.1101/2022.01.09.22268969 (2022).
Li, L. et al. Influenza-associated excess respiratory mortality in China, 2010–15: a population-based study. Lancet Public Health 4, e473–e481 (2019).
United States: Coronavirus Pandemic Country Profile. Our World in Data (19 April 2022); https://ourworldindata.org/coronavirus/country/united-states
Mesfin, Y. et al. Epidemiology of infections with SARS-CoV-2 Omicron BA.2 variant in Hong Kong, January–March 2022. Preprint at medRxiv https://doi.org/10.1101/2022.04.07.22273595 (2022).
Rossman, H. et al. Hospital load and increased COVID-19 related mortality in Israel. Nat. Commun. 12, 1904 (2021).
French, G. et al. Impact of hospital strain on excess deaths during the COVID-19 pandemic – United States, July 2020–July 2021. MMWR Morb. Mortal. Wkly Rep. 70, 1613–1616 (2021).
Mistry, D. et al. Inferring high-resolution human mixing patterns for disease modeling. Nat. Commun. 12, 323 (2021).
Davis, J. T. et al. Cryptic transmission of SARS-CoV-2 and the first COVID-19 wave. Nature 600, 127–132 (2021).
Viner, R. M. et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatrics 175, 143–156 (2021).
Davies, N. G. et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat. Med. 26, 1205–1211 (2020).
Hu, S. et al. Infectivity, susceptibility, and risk factors associated with SARS-CoV-2 transmission under intensive contact tracing in Hunan, China. Nat. Commun. 12, 1533 (2021).
Buitrago-Garcia, D. et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: a living systematic review and meta-analysis. PLoS Med. 17, e1003346 (2020).
Manica, M. et al. Intrinsic generation time of the SARS-CoV-2 Omicron variant: an observational study of household transmission. Preprint at SSRN https://doi.org/10.2139/ssrn.4068368 (2022).
Deng, X. et al. Case fatality risk of the first pandemic wave of novel coronavirus disease 2019 (COVID-19) in China. Clin. Infect. Dis. 73, e79–e85 (2021).
Halloran, M. E., Longini, I. M., Struchiner, C. J. & Longini, I. M. Design and Analysis of Vaccine Studies (Springer, 2010).
Hansen, C. H., Michlmayr, D., Gubbels, S. M., Mølbak, K. & Ethelberg, S. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet 397, 1204–1212 (2021).
Provisional Data Analysis On COVID-19 Reported Death Cases. Center for Health Protection of the Department of Health (29 April 2022); https://www.covidvaccine.gov.hk/pdf/death_analysis.pdf
Statistics on 5th Wave of COVID-19. Center for Health Protection of the Department of Health (29 April 2022); https://www.covidvaccine.gov.hk/pdf/5th_wave_statistics.pdf
Modelling the fifth wave of COVID-19 in Hong Kong. D24H@HKSTP and HKU WHO Collaborating Centre on Infectious Disease Epidemiology and Modelling (21 March 2022); https://sph.hku.hk/en/News-And-Events/Press-Releases/2022/TBC
Guan, W.-j et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382, 1708–1720 (2020).
Modes, M. E. et al. Clinical characteristics and outcomes among adults hospitalized with laboratory-confirmed SARS-CoV-2 infection during periods of B. 1.617. 2 (Delta) and B. 1.1. 529 (Omicron) variant predominance—one hospital, California, July 15–September 23, 2021, and December 21, 2021–January 27, 2022. MMWR Morb. Mortal. Wkly Rep. 71, 217–223 (2022).
Piroth, L. et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respiratory Med. 9, 251–259 (2021).
Rees, E. M. et al. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 18, 270 (2020).
Lefrancq, N. et al. Evolution of outcomes for patients hospitalised during the first 9 months of the SARS-CoV-2 pandemic in France: a retrospective national surveillance data analysis. Lancet Regional Health – Eur. 5, 10087 (2021).
Zhang, J. et al. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study. Lancet Infect. Dis. 20, 793–802 (2020).
Marziano, V. et al. The effect of COVID-19 vaccination in Italy and perspectives for living with the virus. Nat. Commun. 12, 7272 (2021).
Poletti, P. et al. Association of age with likelihood of developing symptoms and critical disease among close contacts exposed to patients with confirmed SARS-CoV-2 infection in Italy. JAMA Netw. Open 4, e211085–e211085 (2021).
Situation Regarding Prevention and Control of COVID-19 Epidemic in Shanghai. Shanghai Municipal Health Commission (29 April 2022); http://wsjkw.sh.gov.cn/xwfbh/index.html
Hart, W. S. et al. Generation time of the alpha and delta SARS-CoV-2 variants: an epidemiological analysis. Lancet Infect. Dis. 22, P603–P610 (2022).
Yang, J. et al. Despite vaccination, China needs non-pharmaceutical interventions to prevent widespread outbreaks of COVID-19 in 2021. Nat. Hum. Behav. 5, 1009–1020 (2021).
Press conference held on situation regarding prevetion and control of COVID-19 epidemics in the coming autumn and winter season and vaccination. The State Council Information Office, P.R.C. (24 October 2021); http://www.gov.cn/xinwen/gwylflkjz169/index.htm
FAQ on booster immunization for COVID-19 vaccines. National Health Commission of China (15 November 2021); http://www.nhc.gov.cn/xcs/s7847/202111/67a59e40580d4b4687b3ed738333f6a9.shtml
Press conference held on situation regarding strict prevetion and control of COVID-19 epidemic. The State Council Information Office, P.R.C. (12 April 2022); http://www.gov.cn/xinwen/gwylflkjz192/index.htm
Relevant requirements on organization and implementation of COVID-19 booster vaccination. National Health Commission of China (17 February 2022); https://m.weibo.cn/status/4737882239533991
Chen, X. et al. Prediction of long-term kinetics of vaccine-elicited neutralizing antibody and time-varying vaccine-specific efficacy against the SARS-CoV-2 Delta variant by clinical endpoint. BMC Med. 20, 36 (2022).
Wang, K. et al. Memory B cell repertoire from triple vaccinees against diverse SARS-CoV-2 variants. Nature 603, 919–925 (2022).
Zhang, Y. et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18-59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 21, 181–192 (2021).
Cao, Y. et al. Humoral immunogenicity and reactogenicity of CoronaVac or ZF2001 booster after two doses of inactivated vaccine. Cell Res. 32, 107–109 (2022).
Pérez-Then, E. et al. Neutralizing antibodies against the SARS-CoV-2 Delta and Omicron variants following heterologous CoronaVac plus BNT162b2 booster vaccination. Nat. Med. 28, 481–485 (2022).
Peiris, M. et al. Neutralizing antibody titres to SARS-CoV-2 Omicron variant and wild-type virus in those with past infection or vaccinated or boosted with mRNA BNT162b2 or inactivated CoronaVac vaccines. Preprint at Res. Sq. https://doi.org/10.21203/rs.3.rs-1207071/v1 (2022).
Cameroni, E. et al. Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shift. Nature 602, 664–670 (2022).
Pfizer’s novel COVID-19 oral antiviral treatment candidate reduced risk of hospitalization or death by 89% in interim analysis of phase 2/3 EPIC-HR study. Pfizer (5 November 2021); https://www.pfizer.com/news/press-release/press-release-detail/pfizers-novel-covid-19-oral-antiviral-treatment-candidate
Acknowledgements
This study was supported by grants from the Key Program of the National Natural Science Foundation of China (82130093). We would like to thank B. J. Cowling, School of Public Health, Li Ka Shing Faculty of Medicine, University of Hong Kong for providing severity parameters. We would also like to thank L. Yi for assistance in figure preparation. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US National Institutes of Health.
Author information
Authors and Affiliations
Contributions
H.Y. conceived, designed and supervised the study. J.C. designed the model. X.D. and H.L. developed the model. J.C., X.D., J.Y., X.C., Q.W., J.Z., W.Z., Z.Z., Z.C., W.L., Y.L. and X.Z. collected the data. K.S. and M.A. contributed to the methodology. X.D. and J.C. analyzed the model output. J.C., X.D., J.Y., K.S., M.A. and H.Y. interpreted the results. Z.C., X.D., C.P., J.C. and R.S. prepared the figures. J.C., J.Y., X.D., Z.C. and H.L. wrote the first draft of the manuscript. M.A. and K.S. critically revised the content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
H.Y. received research funding from Sanofi Pasteur, GlaxoSmithKline, Yichang HEC Changjiang Pharmaceutical Company, Shanghai Roche Pharmaceutical Company and SINOVAC Biotech Ltd. Except for research funding from SINOVAC Biotech Ltd, which is related to the data analysis of clinical trials of immunogenicity and safety of CoronaVac, the others are not related to COVID-19. M.A. has received research funding from Seqirus; the funding is not related to COVID-19. All the other authors have no competing interests.
Peer review
Peer review information
Nature Medicine thanks Gabriel Leung and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Jennifer Sargent, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Model structure flow diagram with transition rates between states.
a, Overview of extended SEIR transmission model. b, Diagram of hospitalization provided symptomatic infections. c, Diagram of antiviral therapies provided symptomatic infections. d, Diagram of vaccination and waning immunity. Note that the complex infection dynamic as shown in a has been encapsulated within a single pink box. All states and parameters are defined in Supplementary Tables 3 and 4.
Extended Data Fig. 2 Comparisons between the observed epidemic curves in Shanghai and model output.
a, Confirmed infections. b, Symptomatic infections. All data are presented as median with 2.5% and 97.5% quantiles of n=200 simulations.
Extended Data Fig. 3 Projected demand and shortage of hospital beds and ICUs for baseline scenario across four settings from March 2022 to September 2022.
a, Daily demand of hospital (non-ICU) beds per 100,000. b, Daily demand of ICU beds per 100,000. In b, the dashed lines indicate the existing number of ICU beds per 100,000 in four settings, and the inset plot shows days of shortage of ICU beds as a function of the number of insufficient ICU beds compared with the capacity of ICU beds in each setting. The curves in the inset are smoothed by B-spline with 8 d.f. China represents the ‘national average’. All data are presented as median with 2.5% and 97.5% quantiles of n=200 simulations.
Extended Data Fig. 4 Projected COVID-19 burden and demands in hospital and ICU beds in China under pessimistic VE scenario compared to the baseline scenario (optimistic VE) from March 2022 to September 2022.
a, Cumulative hospital (non-ICU) admissions. b, Cumulative ICU admissions. c, Cumulative deaths. d, Daily demand in hospital (non-ICU) beds. e, Daily demand in ICU beds. In e, the green dashed line indicates the number of ICU beds available in China. All data are presented as median with 2.5% and 97.5% quantiles of n=200 simulations.
Extended Data Fig. 5 Projected impact of adopting individual mitigation strategies on COVID-19 burden in China under pessimistic VE scenario from March 2022 to September 2022.
a, Cumulative number of hospital (non-ICU) admissions. b, Cumulative number of ICU admissions. c, Cumulative number of deaths. The scenarios indicated on y axis are as follows: subunit vaccines refer to using a third dose of subunit vaccines as booster after two doses of inactivated vaccines as priming. Vaccinating elderly refers to vaccinating approximately 52 million people aged ≥60 years who have not been vaccinated yet as of March 17, 2022. 50% uptake and 80% efficacy corresponds to a scenario where 50% of symptomatic cases receive an antiviral therapy with an efficacy of 80% in preventing hospitalization and death. 100% uptake and 89% efficacy corresponds to a scenario where all symptomatic cases receive an antiviral therapy with an efficacy of 89% in preventing hospitalization and death. School closure corresponds to a scenario where, on the top of baseline strategy, all schools remain closed for the duration of the epidemic. Similarly, school and workplace closure corresponds to a scenario, where on the top of baseline strategy, all schools and workplaces remain closed for the duration of the epidemic. Rt: 3.0, 2.5, and 2.0 correspond to scenarios assuming different levels of NPIs leading to reduced values of the reproduction number. Note that no strict NPIs is implemented in the baseline scenario. All data are presented as median with 2.5% and 97.5% quantiles of n=200 simulations.
Supplementary information
Supplementary Information
Supplementary Tables 1–10 and Figs. 1–7.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cai, J., Deng, X., Yang, J. et al. Modeling transmission of SARS-CoV-2 Omicron in China. Nat Med 28, 1468–1475 (2022). https://doi.org/10.1038/s41591-022-01855-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-022-01855-7
This article is cited by
-
Azvudine versus paxlovid for oral treatment of COVID-19 in Chinese patients
BMC Infectious Diseases (2024)
-
IgG antibody response to SARS-CoV-2 infection and its influencing factors in lymphoma patients
BMC Immunology (2024)
-
Postoperative morbidity and mortality of patients with COVID-19 undergoing cardiovascular surgery: an inverse propensity-weighted study
BMC Anesthesiology (2024)
-
Clinical features that predict the mortality risk in older patients with Omicron pneumonia: the MLWAP score
Internal and Emergency Medicine (2024)
-
Impacts of Vaccination and Severe Acute Respiratory Syndrome Coronavirus 2 Variants Alpha and Delta on Coronavirus Disease 2019 Transmission Dynamics in Four Metropolitan Areas of the United States
Bulletin of Mathematical Biology (2024)