Abstract
Purpose
Hypopituitarism (HP) is an uncommon consequence of Russell’s viper envenomation (RVE). Delayed hypopituitarism (DHP) presents months to years after recovering from snake bites (SB). The clinical presentation, manifestations, and outcomes of DHP following RVE have not been systematically studied. Here, we present a case series of HP following RVE with delayed diagnosis and conduct a literature review.
Methods
We retrospectively reviewed data of eight DHP cases and literature to outline the presentation, manifestations, hormonal profiles, and radiological features of DHP following RVE.
Results
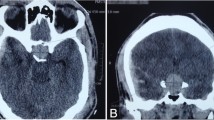
Three men and five women, with a mean age at diagnosis of 39.5 ± 11.6 years, were included. The mean duration between snake bite (SB) and HP diagnosis was 8.1 ± 3.6 years. Secondary hypothyroidism and hypogonadotropic hypogonadism were present in all patients. Growth hormone deficiency (GHD) and secondary hypocortisolism were present in 6 (75%) patients. Magnetic resonance imaging (MRI) revealed empty sella and partially empty sella in three patients each (75%). The literature review revealed additional 20 DHP cases (mean age at diagnosis 32.4 ± 10.8 years), with 65% of patients being men. Fatigue, reduced libido, and loss of weight were the commonest symptoms among men. Secondary amenorrhea, fatigue, and loss of appetite were common manifestations among women. Acute kidney injury, GHD, secondary hypothyroidism, hypogonadism, and adrenal insufficiency were reported in 75%, 79%, 95%, 100%, and 85% of patients, respectively.
Conclusions
DHP is an important complication of RVE, and a delay in its diagnosis is associated with significant morbidity. Patients with RVE should be followed up for a long term to identify DHP.
Similar content being viewed by others
References
Vaiyapuri S, Vaiyapuri R, Ashokan R, Ramasamy K, Nattamaisundar K, Jeyaraj A et al (2013) Snakebite and its socio-economic impact on the rural population of Tamil Nadu, India. PLoS ONE 8(11):e80090
Alirol E, Sharma SK, Bawaskar HS, Kuch U, Chappuis F (2010) Snake bite in South Asia: a review. PLoS Negl Trop Dis 4(1):e603
Mohapatra B, Warrell DA, Suraweera W et al (2011) Snakebite mortality in India: a nationally representative mortality survey. PLoS Negl Trop Dis 5(4):e1018. https://doi.org/10.1371/journal.pntd.0001018
Warrell DA, Gutiérrez JM, Calvete JJ, Williams D (2013) New approaches & technologies of venomics to meet the challenge of human envenoming by snakebites in India. Indian J Med Res 138(1):38–59
Mehta S, Sashindran V (2002) Clinical features and management of snake bite. Med J Armed Forces India 58(3):247–249. https://doi.org/10.1016/S0377-1237(02)80140-X
Ahmed SM, Ahmed M, Nadeem A, Mahajan J, Choudhary A, Pal J (2008) Emergency treatment of a snake bite: pearls from literature. J Emerg Trauma Shock 1(2):97–105. https://doi.org/10.4103/0974-2700.43190
Eapen CK, Chandy N, Kochuovarkey KL et al (1976) Unusual complication of snake bite: hypopituitarism after viper bites. In: Ohsaka A, Hayashi K, Sawai Y (eds) Animal, plant and microbial toxins, vol 2. Plenum Press, New York, pp 467–473
Tun-Pe, Phillips RE, Warrell DA, Moore RA, Tin-Nu-Swe, Myint-Lwin, Burke CW (1987) Acute and chronic pituitary failure resembling Sheehan’s syndrome following bites by Russell’s viper in Burma. Lancet 2(8562):763–767
Rajagopala S, Thabah MM, Ariga KK, Gopalakrishnan M (2015) Acute hypopituitarism complicating Russell’s viper envenomation: case series and systematic review. QJM 108(9):719–728. https://doi.org/10.1093/qjmed/hcv011
Antonypillai CN, Wass JA, Warrell DA, Rajaratnam HN (2011) Hypopituitarism following envenoming by Russell’s vipers (Daboia siamensis and D. russelii) resembling Sheehan’s syndrome: first case report from Sri Lanka, a review of the literature and recommendations for endocrine management. QJM 104(2):97–108. https://doi.org/10.1093/qjmed/hcq214
Golay V, Roychowdhary A, Dasgupta S, Pandey R (2014) Hypopituitarism in patients with vasculotoxic snake bite envenomation related acute kidney injury: a prospective study on the prevalence and outcomes of this complication. Pituitary 17(2):125–131. https://doi.org/10.1007/s11102-013-0477-1
James E, Kelkar PN (2001) Hypopituitarism after viperine bite. J Assoc Phys India 49:937–938
Srinivasan KG, Srividya S, Usha Nandhini KP, Ramprabananth S (2010) Chronic pituitary failure resembling Sheehan’s syndrome following a bite of Russell’s viper. A case report. Neuroradiol J 23(1):38–41
Bandyopadhyay SK, Bandyopadhyay R, Dutta A, Pal SK (2012) Hypopituitarism following poisonous viperbite. J Indian Med Assoc 110(2):120–122
Prabhakar A, Gupta V, Bhansali A, Vyas S, Khandelwal N (2013) Hypopitutarism secondary to snake envenomation. Neurol India 61:310–311
Kamath AT, Satish Kumar S (2013) Snake bite and hypopituitarism: ignorance or incompetence? Endocr Abs 31:1–1
Golay V, Roychowdhary A, Pandey R, Pasari A, Praveen M, Arora P, Sarkar D (2013) Growth retardation due to panhypopituitarism and central diabetes insipidus following Russell’s viper bite. Southeast Asian J Trop Med Public Health 44(4):697–702
Grace M, Shanoj KC (2014) An unusual complication of snake bite. Egypt J Intern Med 26:91–92
Chakrabarti S (2014) Snake-Bite induced panhypopituitarism—an uncommon scenario. Indian J Med Case Rep 3:1–3
Shetty S, Abi MS, Hickson R, David T, Rajaratnam S (2014) Hypopituitarism and autoimmune thyroiditis following snake bite: an unusual clinical scenario. J Assoc Phys India 62(11):55–57
Sudulagunta SR, Sodalagunta MB, Khorram H, Sepehrar M, Noroozpour Z (2015) Generalized fatigue, amenorrhea due to snake bite? SM J Case Rep 1(1):1002
Ratnakaran B, Punnoose VP, Das S, Kartha A (2016) Psychosis in secondary empty sella syndrome following a Russell’s viper bite. Indian J Psychol Med 38(3):254–256
Amalnath D, Baskar D (2016) Multiple endocrine gland apoplexy post-snake bite. JCR 6:479–481
Majumdar R, Mukherjee L, Biswas U, Jana CK (2017) Pituitary apoplexy—a rare and unusual complication following viper bite. Int J Med Sci Public Health 6:429–431
Shivaprasad C (2011) Sheehan’s syndrome: newer advances. Indian J Endocrinol Metab 15(Suppl 3):S203–S207
Isbister GK, Maduwage K, Scorgie FE, Shahmy S, Mohamed F, Abeysinghe C, Karunathilake H, O’Leary MA, Gnanathasan CA, Lincz LF (2015) Venom concentrations and clotting factor levels in a prospective cohort of Russell’s viper bites with coagulopathy. PLoS Negl Trop Dis 9(8):e0003968
Than-Than, Francis N, Tin-Nu-Swe, Myint-Lwin, Tun-Pe, Soe-Soe, Maung-Maung-Oo, Phillips RE, Warrell DA (1989) Contribution of focal haemorrhage and microvascular fibrin deposition to fatal envenoming by Russell’s viper (Vipera russelli siamensis) in Burma. Acta Trop 46(1):23–38
Proby C, Tha-Aung, Thet-Win, Hla-Mon, Burrin JM, Joplin GF (1990) Immediate and long-term effects on hormone levels following bites by the Burmese Russell’s viper. Q JMed 75:399–411
Warrell DA (2009) Researching nature’s venoms and poisons. Trans R Soc Trop Med Hyg 103:860–866
Goswami R, Kochupillai N, Crock PA, Jaleel A, Gupta N (2002) Pituitary autoimmunity in patients with Sheehan’s syndrome. J Clin Endocrinol Metab 87(9):4137–4141
De Bellis A, Kelestimur F, Sinisi AA, Ruocco G, Tirelli G, Battaglia M et al (2008) Anti-hypothalamus and anti-pituitary antibodies may contribute to perpetuate the hypopituitarism in patients with Sheehan’s syndrome. Eur J Endocrinol 158(2):147–152
Wolff H (1958) Insuficiência hipofisária anterior por picada de ofídio. Arq Bras Endocrinol Metabol 7:25–47
Casewell NR, Wagstaff SC, Wüster W, Cook DA, Bolton FM, King SI, Pla D, Sanz L, Calvete JJ, Harrison RA (2014) Medically important differences in snake venom composition are dictated by distinct postgenomic mechanisms. Proc Natl Acad Sci USA 111(25):9205–9210
Rosén T, Bengtsson BA (1990) Premature mortality due to cardiovascular disease in hypopituitarism. Lancet 336(8710):285–288
Bates AS, Van’t Hoff W, Jones PJ, Clayton RN (1996) The effect of hypopituitarism on life expectancy. J Clin Endocrinol Metab 81(3):1169–1172
Prabhakar VKB, Shalet SM (2006) Aetiology, diagnosis, and management of hypopituitarism in adult life. Postgrad Med J 82(966):259–266
Tomlinson JW, Holden N, Hills RK, Wheatley K, Clayton RN, Bates AS, Sheppard MC, Stewart PM (2001) Association between premature mortality and hypopituitarism. West Midlands Prospective Hypopituitary Study Group. Lancet 357(9254):425–431
Bengtsson BA (1998) Untreated growth hormone deficiency explains premature mortality in patients with hypopituitarism. Growth Horm IGF Res 8(Suppl A):77–80
Crespo I, Santos A, Webb SM (2015) Quality of life in patients with hypopituitarism. Curr Opin Endocrinol Diabetes Obes 22(4):306–312
Hall R, Manski-Nankervis J, Goni N, Davies MC, Conway GS (2006) Fertility outcomes in women with hypopituitarism. Clin Endocrinol (Oxford) 65(1):71–74
Acknowledgements
We would like to acknowledge the timely help provided by Dr. Nagashree N, Intern Medical Officer at the Vydehi Institute of Medical Sciences and Research Centre in retrieving full text manuscripts. We would also like to thank Mrs. Sumithra Selvan for her help in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shivaprasad, C., Aiswarya, Y., Sridevi, A. et al. Delayed hypopituitarism following Russell’s viper envenomation: a case series and literature review. Pituitary 22, 4–12 (2019). https://doi.org/10.1007/s11102-018-0915-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-018-0915-1