Dementia: assessment, management and support: summary of updated NICE guidance
BMJ 2018; 361 doi: https://doi.org/10.1136/bmj.k2438 (Published 20 June 2018) Cite this as: BMJ 2018;361:k2438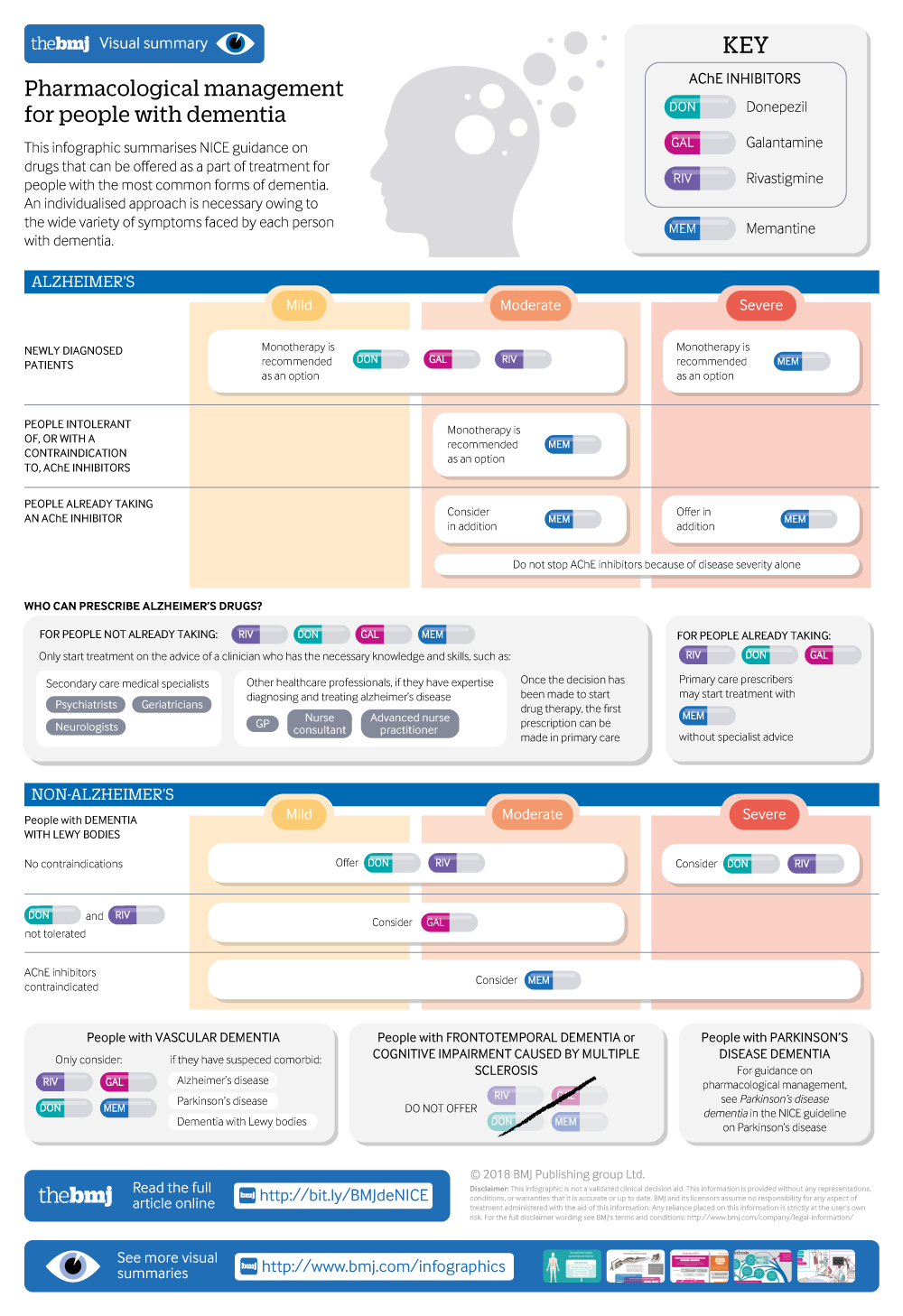
Visual summary available
Pharmaceutical management of dementia, including Alzheimer's disease, dementia with lewy bodies, vascular dementia, frontotemporal dementia, and cognitive impairment caused by multiple sclerosis.
- Joshua Pink, technical adviser1,
- John O’Brien, professor of old age psychiatry2,
- Louise Robinson, professor of primary care and ageing3,
- Damien Longson, consultant liaison psychiatrist, chair of Guideline Committee4
- on behalf of the Guideline Committee
- 1National Institute for Health and Care Excellence, Manchester M1 4BT, UK
- 2Department of Psychiatry, University of Cambridge, Cambridge Biomedical Campus, Cambridge CB2 0SP, UK
- 3Newcastle University Institute for Ageing and Institute for Health & Society, Newcastle University, Newcastle Biomedical Research Building, Campus for Ageing and Vitality, Newcastle upon Tyne NE4 5PL, UK
- 4Greater Manchester Mental Health Foundation Trust, Bury New Road, Prestwich, Manchester M25 3BL, UK
- Correspondence to: J Pink joshua.pink{at}nice.org.uk
What you need to know
When using cognitive testing in primary care, use brief, validated tools such as 10 point cognitive screener (10-CS) or 6 item cognitive impairment test (6CIT) rather than longer tests such as the MMSE
People living with dementia should be provided with a single health or social care professional to coordinate their care
For people with mild to moderate dementia, offer group cognitive stimulation therapy but not cognitive training
High anticholinergic burden can lead to cognitive impairment, thereby worsening the cognitive symptoms of dementia or causing false positive diagnoses: validated tools, such as the Anticholinergic Cognitive Burden Scale, can determine whether this is an issue
Inform carers of people living with dementia that they are entitled to a formal needs assessment and assessment for respite and should be offered access to psychoeducation and skills training
Dementia describes a range of cognitive, behavioural, and psychological symptoms that can include memory loss, problems with reasoning and communication, and change in personality which impair a person’s ability to carry out daily activities.
A report published by the Alzheimer’s Society in 2013 found there were about 815 000 people living with dementia in the UK (corresponding to a prevalence of 1 in 14 in people over 65 years old), and this number is expected to increase to 1 143 000 by 2025.1 In November 2017, there were 456 739 people on general practice registers with a formal diagnosis of dementia, up from approximately 290 000 people in 2009-10,2 with most of this difference accounted for by an increase in diagnosis rates. Despite this improvement in diagnosis, around 1 in 3 people with established dementia remain unrecognised, and around half of people living with dementia in England do not feel they are getting sufficient post-diagnostic support.3
This article summarises the most recent recommendations from the National Institute for …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £173 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£38 / $45 / €42 (excludes VAT)
You can download a PDF version for your personal record.
