Intended for healthcare professionals
Rapid response to:
Practice
Clinical Updates
Pregnancy in women with congenital heart disease
BMJ 2018; 360 doi: https://doi.org/10.1136/bmj.k478 (Published 09 March 2018) Cite this as: BMJ 2018;360:k478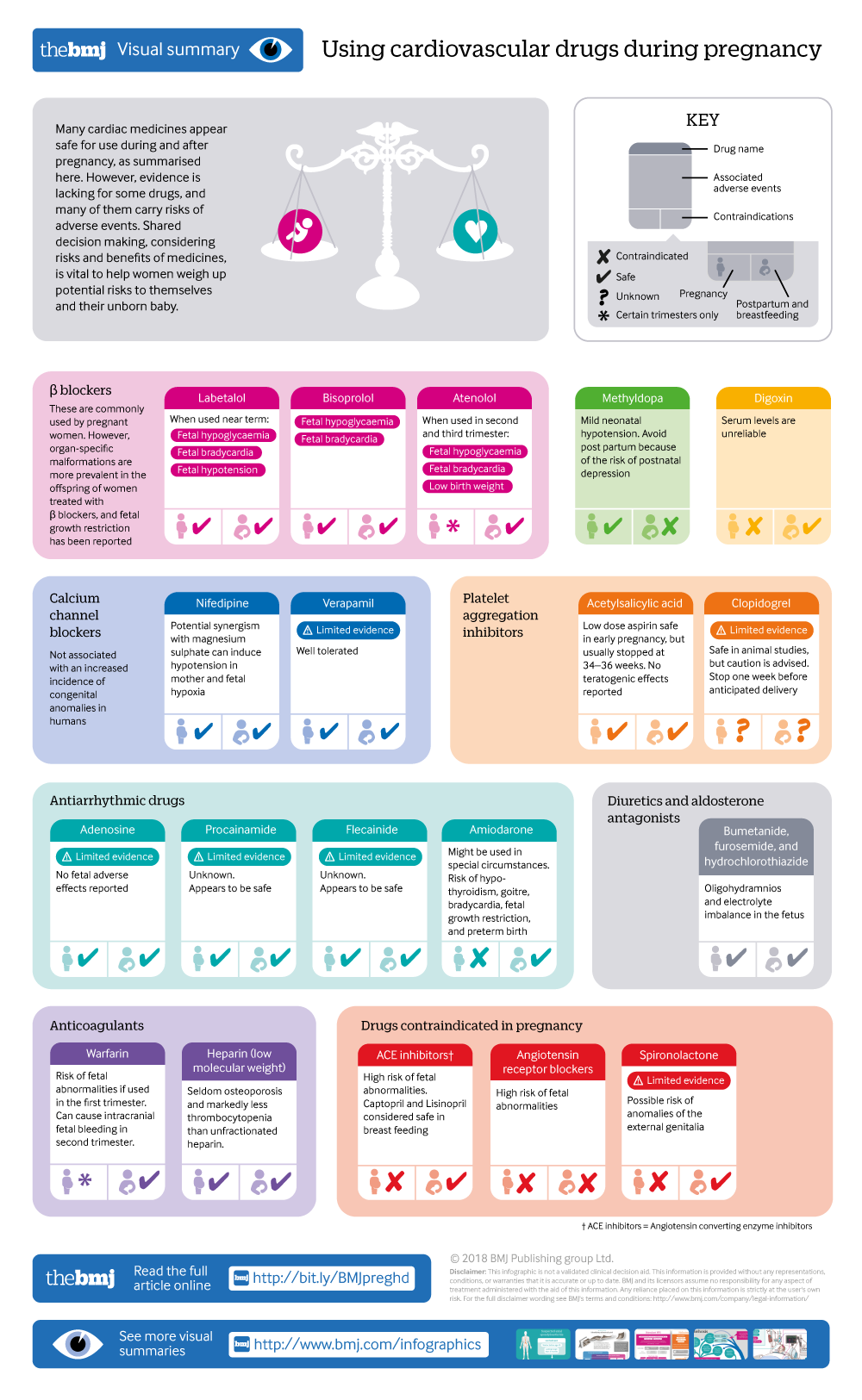
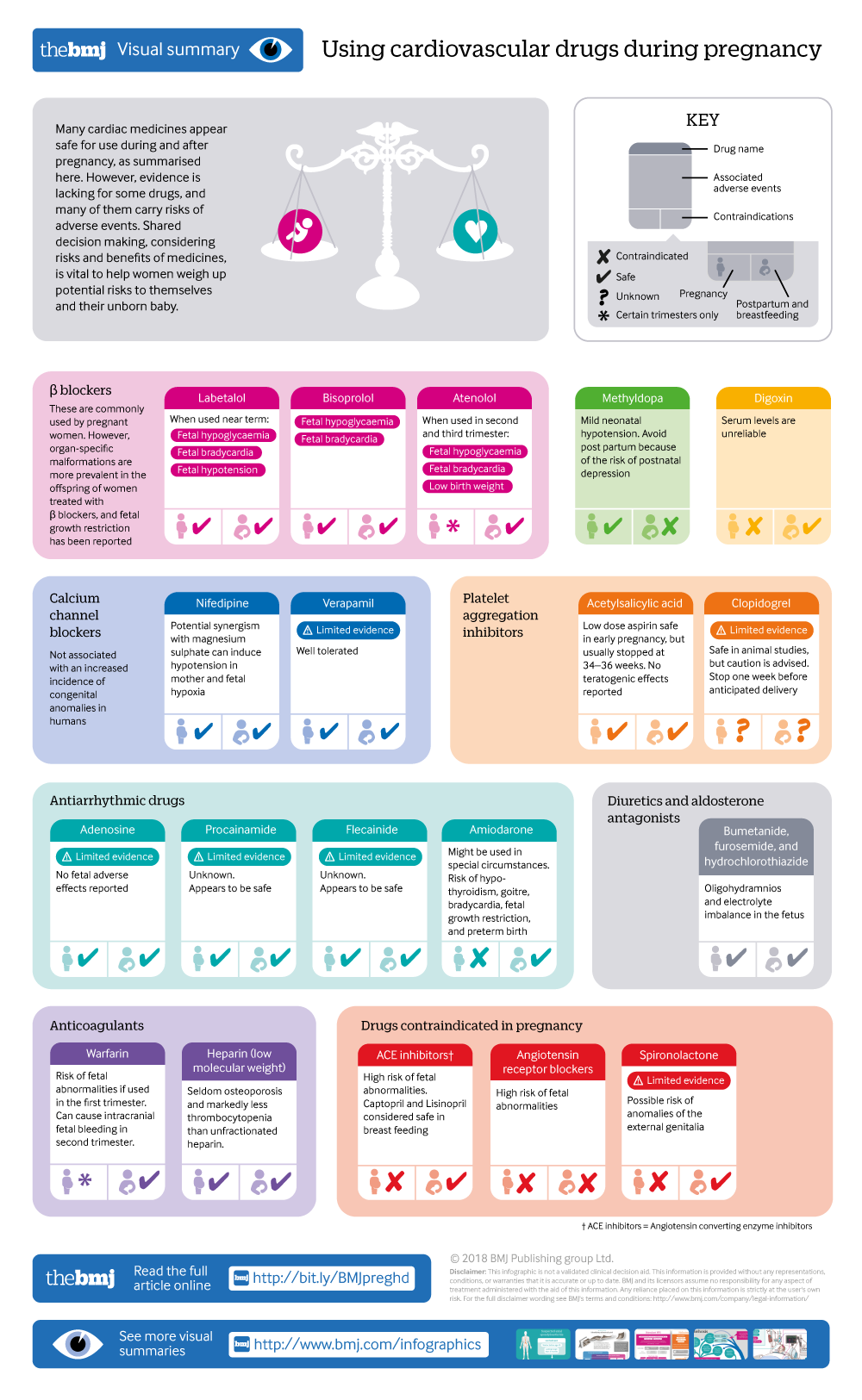
Using cardiovascular drugs during pregnancy
An approach
Rapid Response:
Re: Pregnancy in women with congenital heart disease
The recent update by Cauldwell et al provides an excellent overview on managing pregnancy in women with congenital heart disease. They highlight the European Society of Cardiology (ESC) recommendation that women with a modified World Health Organization (mWHO) cardiovascular disease risk as III or IV should receive specialist antenatal care (1). In the UK, this is available in only 14 centres, usually in tertiary settings. However, this may not be the best option for women that do not live near a tertiary centre. In a remote area like Cornwall, this involves pregnant women travelling approximately 300 miles to Bristol for consultations and delivery. Given the unpredictable nature of delivery, this can involve lengthy stays away from their families.
To address this, a joint service was set up at the Royal Cornwall Hospitals Trust (RCHT) between a visiting congenital heart disease specialist from Bristol and a local obstetrician which included a multidisciplinary cardiac obstetric clinic as recommended by the ESC. The cases were also discussed in a monthly MDT discussion with Bristol and a comprehensive care plan for the rest of pregnancy and delivery were formulated. We reviewed the cases of 30 women who had attended the clinic between 2011 and 2016. The majority of the women were classified into the mWHO class II-III. The mode number of visits to the combined clinic was two, and 80% of the patients delivered at the RCHT. Encouragingly none of the patients who delivered at the RCHT had a major maternal and neonatal complication and the majority delivered vaginally and received lumbar epidural anaesthesia as recommended. A survey of service-users at one clinic in 2016 (n=10) revealed all of the patients would rather have their maternal care locally, in fact one patient said that even the RCHT was a long way to travel. This innovative approach ensures women have access to highly specialised care whilst minimising travel burden.
References
1. Regitz-Zagrosek V., Lundqvist C. B., Borghi C. Cifkova R., Ferriera R., Foidart JM., et al. ESC guidelines on the management of cardiovascular diseases during pregnancy: The Task Force on the Management of Cardiovascular Diseases During Pregnancy of the European Society of Cardiology (ESC) Eur Heart J. 2011. 32(24):3147–3197.
Competing interests: No competing interests