Assessment of child or young person with a possible eating disorder
BMJ 2017; 359 doi: https://doi.org/10.1136/bmj.j5328 (Published 07 December 2017) Cite this as: BMJ 2017;359:j5328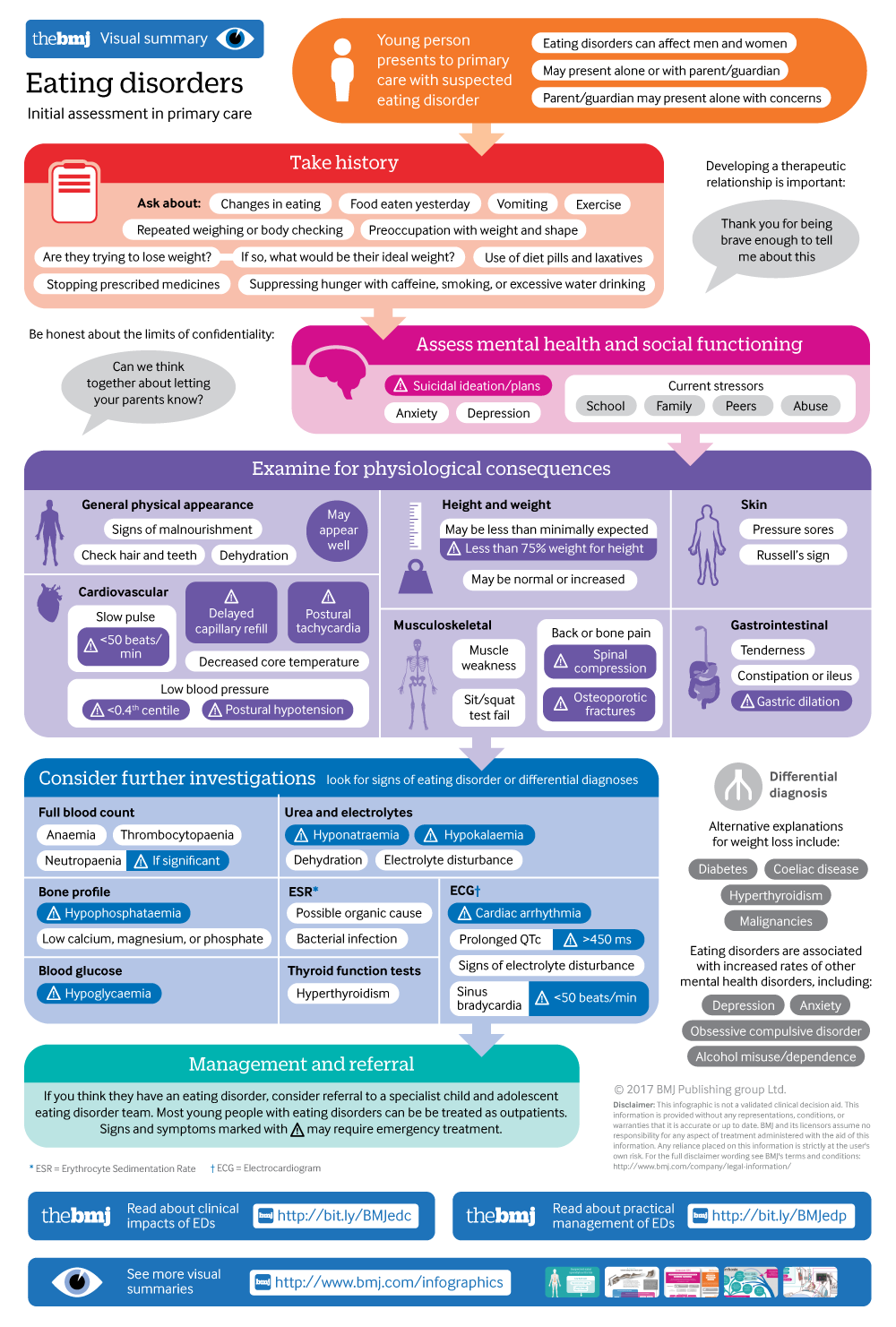
Infographic available
Click here for a visual overview of initial assessment of eating disorders in primary care.
- Helen Bould, Wellcome Doctoral Training Fellow and specialty training registrar in child and adolescent psychiatry1,
- Claudia Newbegin, general practitioner3,
- Mina Fazel, associate professor of child and adolescent psychiatry and consultant child and adolescent psychiatrist1,
- Anne Stewart, consultant child and adolescent psychiatrist, joint clinical lead for Oxon and Bucks CAMHS eating disorder service and honorary senior clinical lecturer2,
- Alan Stein, professor of child and adolescent psychiatry1
- 1Department of Psychiatry, Warneford Hospital, Oxford, UK
- 2Raglan House, Oxford, UK
- 3Park Medical Group, Newcastle Upon Tyne, UK
- Correspondence to H Bould helen.bould{at}psych.ox.ac.uk
What you need to know
When a child or young person presents alone, it is important to be honest with them from the start about the limits of confidentiality
Parents can become used to the “new normal” of disordered eating; it is important to explain the risks
Focus ideas about treatment on helping the young person feel better about themselves rather than particularly on their weight
A mother presents to discuss her 13 year old daughter’s changed eating patterns. The daughter is involved in a lot of sport at school and is running cross country for the county, but is no longer eating properly and seems withdrawn. The daughter appears to be losing weight, but she does not want to be weighed and alludes to thinking she is fat. She doesn’t know her mother has come to see you; the mother wants to know what she can do without you seeing her daughter, as she is worried her daughter will become upset and withdrawn if others are involved.
Assessing young people with possible eating disorders can be complex for a variety of reasons. Building a therapeutic relationship with a young person with a possible eating disorder and their family is key to enabling a thorough assessment and ongoing management, but it introduces difficult issues regarding confidentiality and risk. This Practice Pointer is aimed at non-specialist doctors and will offer advice on building therapeutic relationships in consultation with a child or young person, and with their parent(s), what information to gather, and how to do so sensitively, and the role of the parent or carer in treatment. We recommend that it is read alongside the accompanying Clinical Update for the evidence base and detailed notes on examination, investigations, when to refer, and risk. The advice in this Practice Pointer is based on expert experience.
Developing the therapeutic relationship
An approach to a young person and parent/carer presenting together
Sensitive information gathering
The most …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £173 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£38 / $45 / €42 (excludes VAT)
You can download a PDF version for your personal record.
