Intended for healthcare professionals
Rapid response to:
Practice
Practice Pointer
Primary care management of postoperative shoulder, hip, and knee arthroplasty
BMJ 2017; 359 doi: https://doi.org/10.1136/bmj.j4431 (Published 18 October 2017) Cite this as: BMJ 2017;359:j4431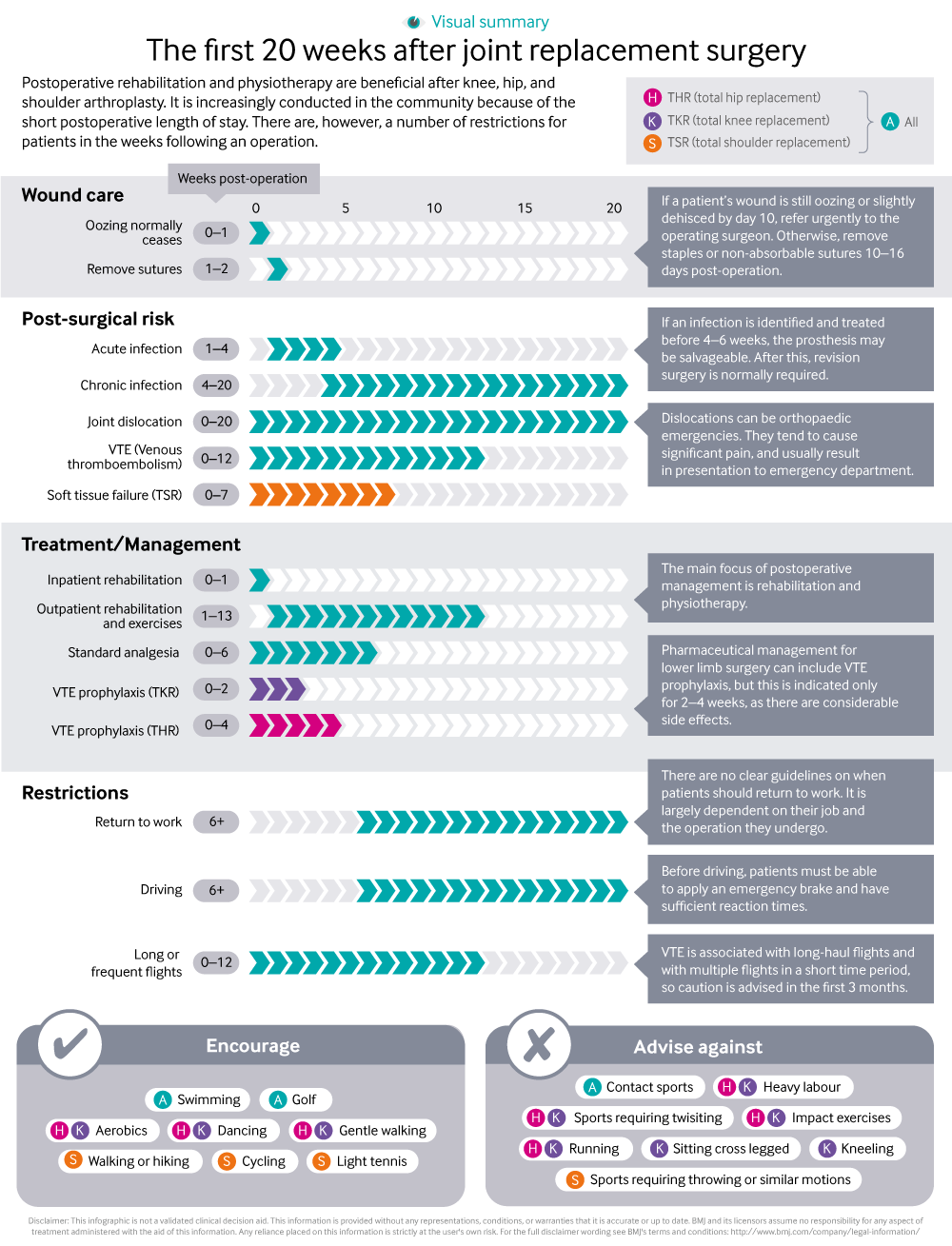
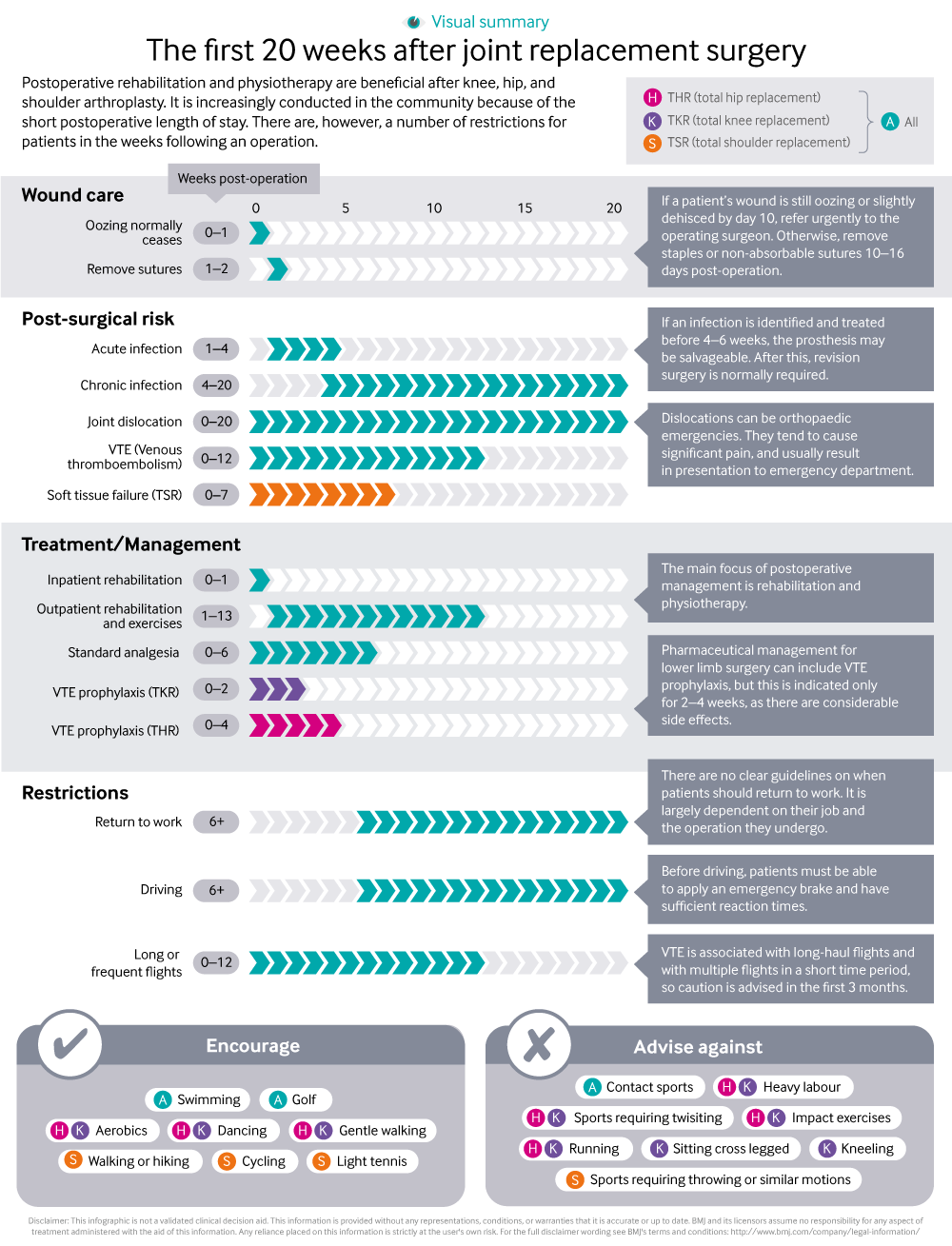
Infographic available
A visual summary of management and restrictions for people following joint replacement surgery.
Rapid Response:
Re: Primary care management of postoperative shoulder, hip, and knee arthroplasty
A few points
1. Do the authors ensure that (unexpected events apart) the SAME physiotherapist carries out preop assessment and education of the patient AND post-op care?
It seems self-evident that this is far better than different physios preop and postop.
2. Can the authors give data for wound dehiscence - a) after sutures, b) after clips?
Where dehiscence did occur, was it because of poor nutritional state
OR
Poor technique? (inadvertent inversion of wound edges)
3. Here I ask Mr Alam and colleagues -
Why should a clean ORTHOPAEDIC wound require preop antibiotics?
If the fear is that circulating bacteria in the blood might decide to find a “nest” in the raw bones or indeed in the surgically damaged tissues (a perfectly reasonable scenario) then it seems reasonable to continue the antibiotic for 48 hours post-op.
4. I ask the authors and Mr Alam and his colleagues -
Surely the GP (educated in the UK, or in a reputable medical school abroad, or having spent six months working in orthopaedics or in general surgery) should be considered capable of FIRST taking a swab ftom the oozing site, SECOND, starting antibiotics IF he/she condiders necessary and then, THIRD, referring the patient straightaway to the Team which operated upon him/her.
I would appreciate replies on the points raised.
Competing interests: No competing interests