Intended for healthcare professionals
Rapid response to:
Practice
Practice Pointer
Primary care management of postoperative shoulder, hip, and knee arthroplasty
BMJ 2017; 359 doi: https://doi.org/10.1136/bmj.j4431 (Published 18 October 2017) Cite this as: BMJ 2017;359:j4431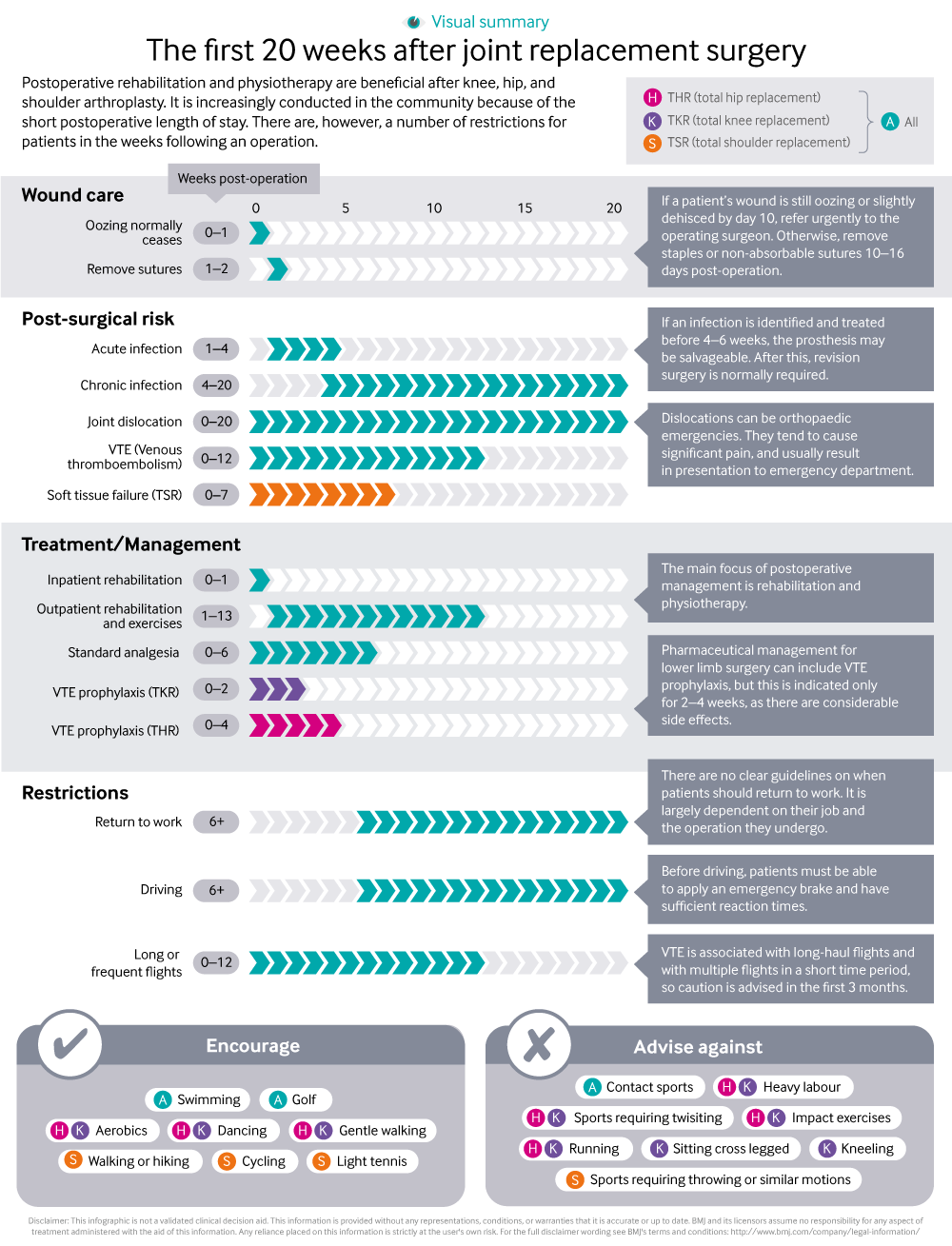
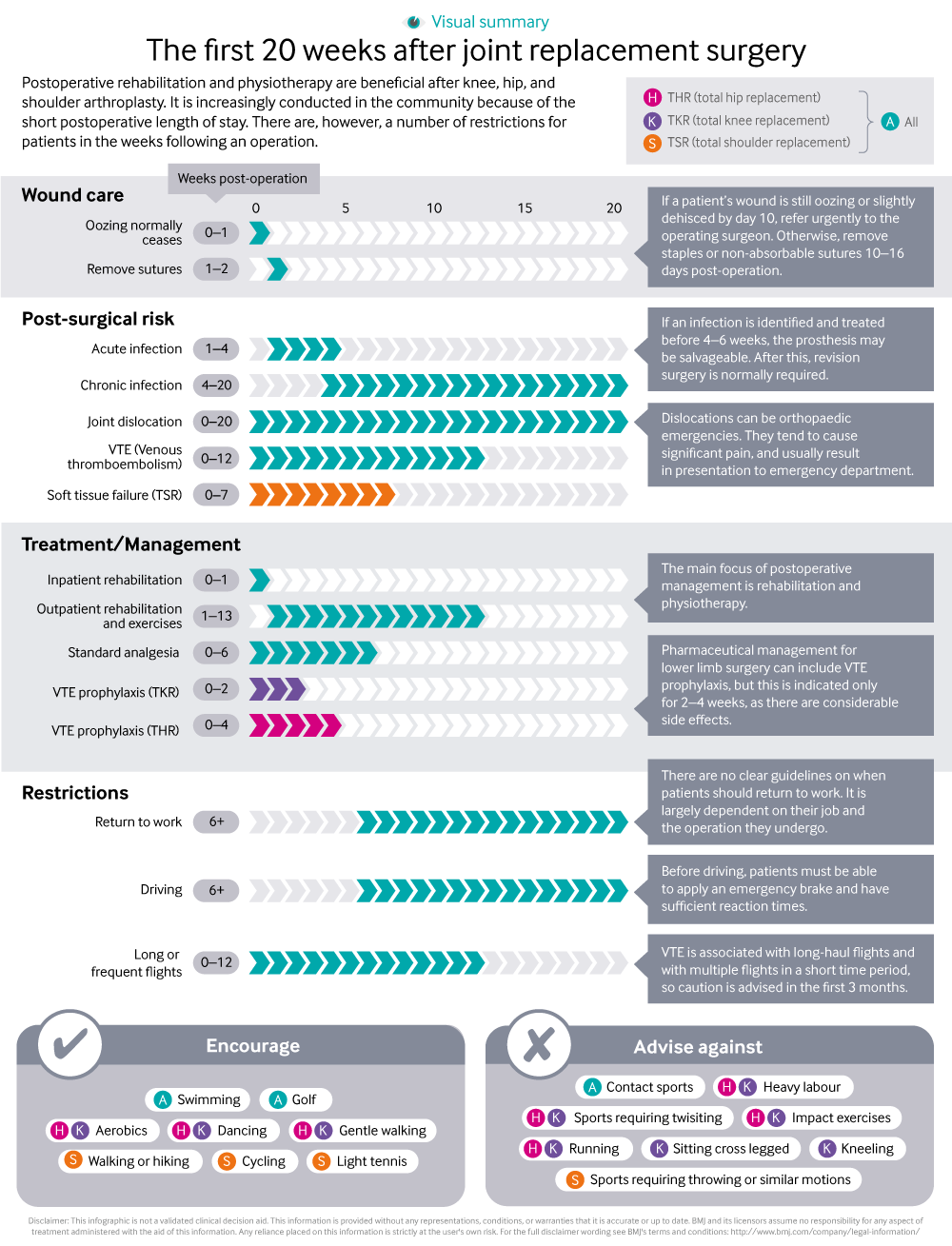
Infographic available
A visual summary of management and restrictions for people following joint replacement surgery.
Rapid Response:
Re: Primary care management of postoperative shoulder, hip, and knee arthroplasty
Dear Sir
We found the ‘Practice Pointer’ by Aresti et al on Postoperative management of shoulder, hip or knee arthroplasty very useful in explaining what to expect in the first 20 weeks after joint replacement, especially the infographic. 1
For the past three years, we have been running a multidisciplinary team meeting (MDT) to review and advise on the management of bone and joint infections including those following joint replacement surgery. As the patients are discharged very soon after surgery (< 5 days) many of the infections become apparent in the community. These patients are seen by GPs or community nurses. In our experience, some of the GPs and nurses have made an incorrect diagnosis of infection in the immediate postoperative period based on presence of redness and oozing of serosanguinous fluid from the wound. Invariably these patients are commenced on antibiotics, often without taking wound swabs.
In England, all NHS hospitals performing joint replacement surgery are mandated to report surgical site infections (SSI) occurring within a month of the surgery. As a result of infection being identified in self-completion post-discharge surveillance questionnaires, we recently reviewed three patients who were diagnosed and treated for superficial SSI of knee arthroplasty in the community. On review, two of the patients did not have any evidence of infection at the time of diagnosis and one had prolonged oozing, without other signs of infection. All three had fully healed wounds one month after surgery. Incorrect diagnosis of postoperative infection has implications for the patient (anxiety and unnecessary antibiotic treatment) and the organisation (misleading infection rates).
We have recently developed a care pathway where GPs and community nurses are advised not to treat cases of suspected postoperative infection of arthroplasty but to urgently refer to a nurse in the orthopaedic department. The nurse assesses the patient and refers to an orthopaedic surgeon if she suspects an infection.
Competing interests: No competing interests