Intended for healthcare professionals
Rapid response to:
Practice
Practice Pointer
Indications for anticoagulant and antiplatelet combined therapy
BMJ 2017; 359 doi: https://doi.org/10.1136/bmj.j3782 (Published 05 October 2017) Cite this as: BMJ 2017;359:j3782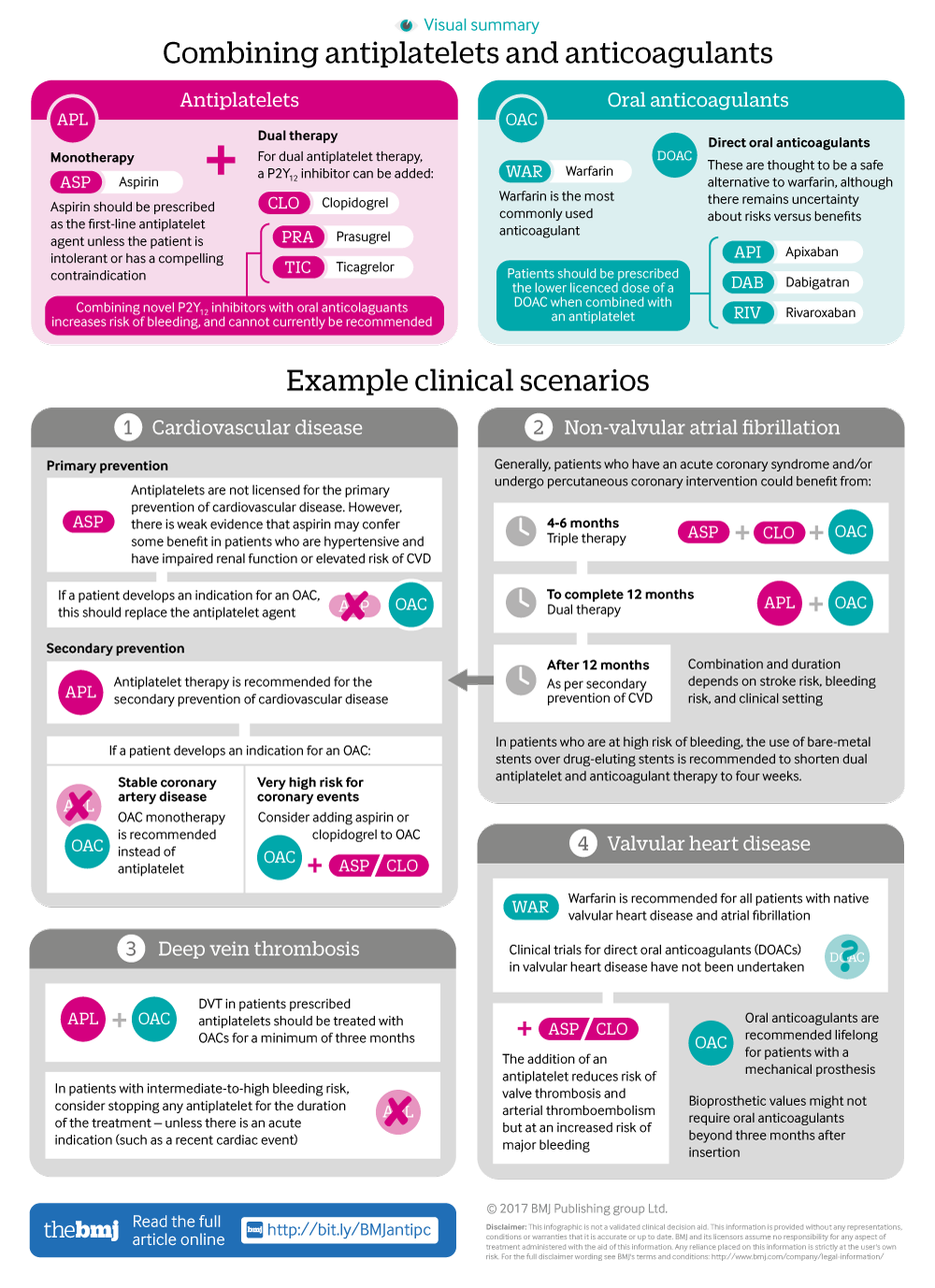
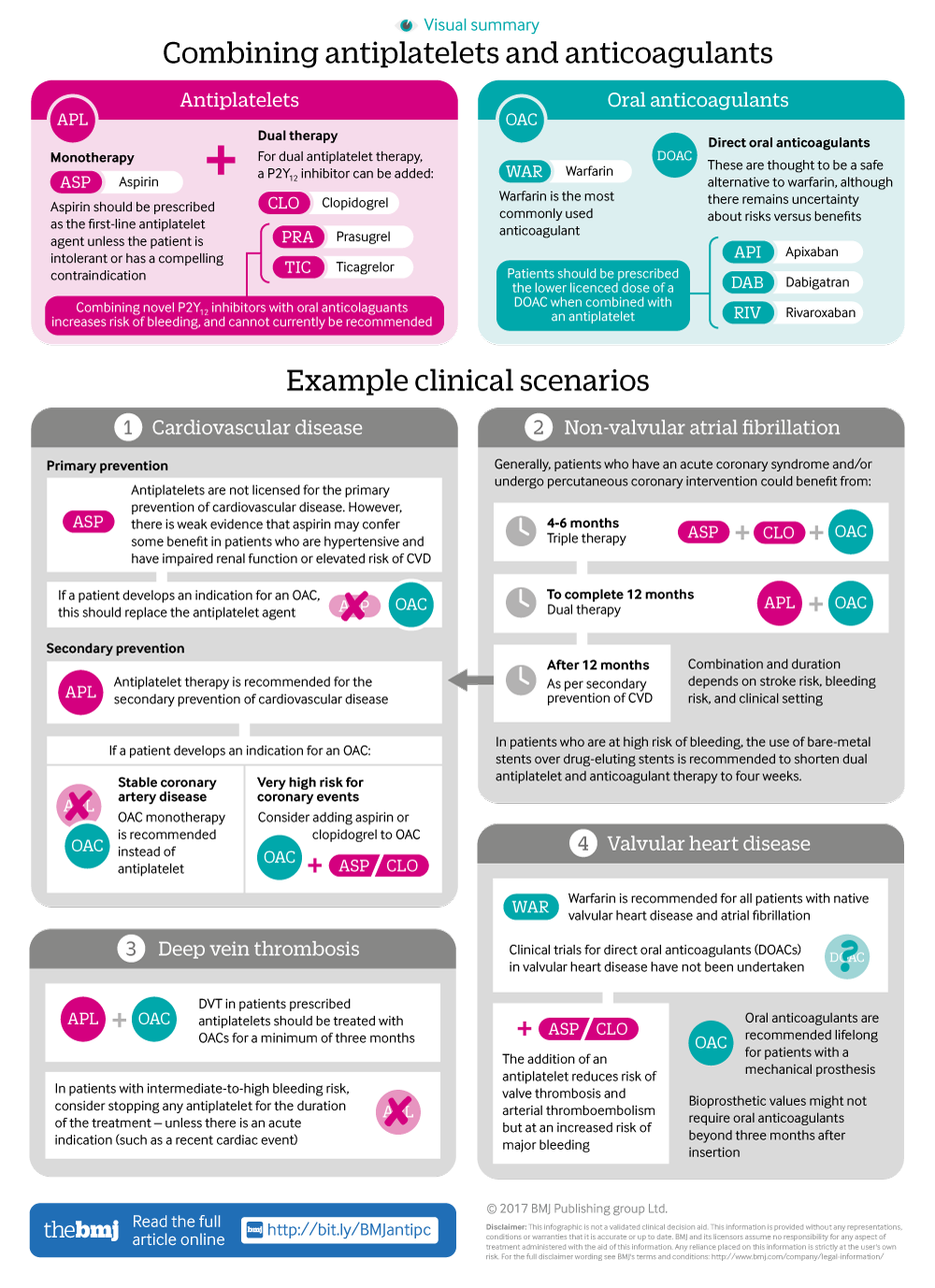
Infographic available
A visual summary of approaches for combining anticoagulants and antiplatelets, along with clinical scenario examples
Rapid Response:
Authors' reply to Julia Kuczynska
We thank Kuczynska for highlighting the European Society of Cardiology update on the use of dual antiplatelet therapy [1]. The recommendations were published after the acceptance of our manuscript and were therefore not considered during its drafting. The update does however contain a number of points that are relevant to our Practice Pointer considering the combination of antiplatelet and anticoagulant therapy [2].
In patients with an indication for oral anticoagulation undergoing percutaneous coronary intervention, the duration and choice of antithrombotic therapy are largely the same as previous recommendations. An absence of safety and efficacy data mean that the use of prasugrel and ticagrelor in triple therapy should still be avoided. Similarly, in patient treated with warfarin a target INR in the lower part of the recommended range should be considered, and in patients treated with a direct oral anticoagulant the ‘lowest effective tested dose for stroke prevention’ should be considered [1].
The recommendation for choice of stent in patients with a high bleeding risk who require long-term anticoagulation has been updated as indicated by Kuczynska. Data from the DAPT trial and others has indicated that second generation drug-eluting stents are superior to bare metal stents where antithrombotic therapy needs to be terminated [4,5]. Second generation drug-eluting stents should therefore be the ‘default choice in patients with high bleeding risk’ [1].
1. Valgimigli M, et al. Eur Heart J 2017; 0, 1–48
2. Floyd CN and Ferro A. BMJ 2017;359:j3782
3. Lip GY , Windecker S, Huber K et al. Eur Heart J 2014; 359:3155-79
4. Kereiakes DJ, et al. JAMA. 2015 Mar 17;313(11):1113-21
Competing interests: No competing interests