Intended for healthcare professionals
Rapid response to:
Practice
Practice Pointer

Exploring thoughts of suicide
BMJ 2017; 356 doi: https://doi.org/10.1136/bmj.j1128 (Published 30 March 2017) Cite this as: BMJ 2017;356:j1128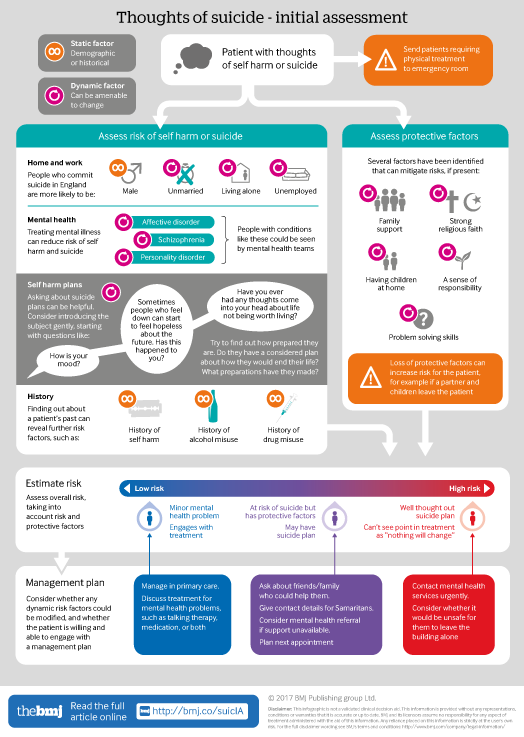
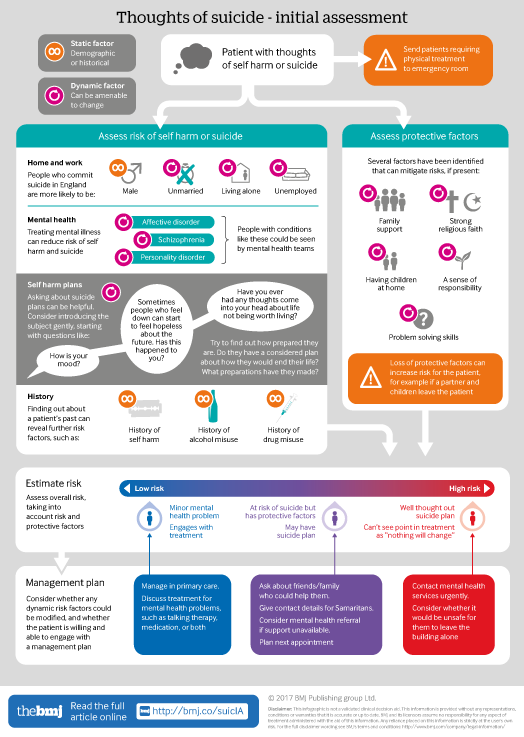
Infographic available
Click here for a visual overview of initial assessment for patients having suicidal thoughts. Includes risk and protective factors that need to be balanced to determine a patient's overall risk of suicide.

Rapid Response:
Re: Exploring thoughts of suicide
The infographic is a helpful way for clinicians in primary and secondary care to understand risk factors for suicide. Alcohol and drug dependence are historical static risk factors in that previous dependence or harmful use increases risk. However it is also best understood as a dynamic risk factor as well. Indeed , it is one of the most significant dynamic risk factors regarding risk of self harm and completed suicide.
For example, if a patient with suicidal thoughts is using alcohol to cope with depression and social / psychological distress, this will increase the risk of completed suicide by all means. When caring for someone in this position, this dynamic risk will be lessened it we are able to support the patient to access services to address this need. Practical advice and motivationally orientated assessment will help in this and reduce risk if successful. This also allows a greater chance that other means of help ( such as antidepressant medication or talking therapy, not to mention patient's personal resources) will be successful. So it is important that clinicians involved with a patient's care understand the dynamic nature of this risk and that it can be reduced with appropriate support.
Regarding prescribed medication such as benzodiazepine and opiates, they deserve some attention in understanding the risk of suicide. It may be that the prescription of benzodiazepines is appropriate despite the increased risk. However understanding that when combined with alcohol and taken in excess, research suggests that this will increase the risk. Being mindful of this allows discussion with patients to educate them of these risk factors and to take steps to address them. There is a dose relationship with risk, so if a patient is on diazepam 40mg daily and suffering from self harm, reducing to 30mg may reduce the risk and so on. If prescriptions are collected for a 1 month period, reducing this to a shorter period, such as a week, could reduce the risk. If prescriptions are being used up 'early', this amounts to a de facto increased dose if new prescriptions are issued, an agreement can be arrived at with the patient to plan that early prescriptions will not be automatically issued, protecting patients from escalating doses that were not envisioned or planned for clinically.
If a patient is taking overdoses whilst using benzodiazepines with binge use of alcohol, the prescriber could review the risks of this prescription against the benefits, to inform a decision as to whether they support the ongoing prescription . An agreement can be reached with the patient to protect them from this risk by reducing and stopping the prescription in an appropriate collaborative manner.
Similar strategies can apply to opiates as well, and understanding that co-prescription of opiates and benzodiazepines is a risk factor in of itself also helps to stratify risks.
Competing interests: No competing interests