Intended for healthcare professionals
Rapid response to:
Practice
Guidelines
Low back pain and sciatica: summary of NICE guidance
BMJ 2017; 356 doi: https://doi.org/10.1136/bmj.i6748 (Published 06 January 2017) Cite this as: BMJ 2017;356:i6748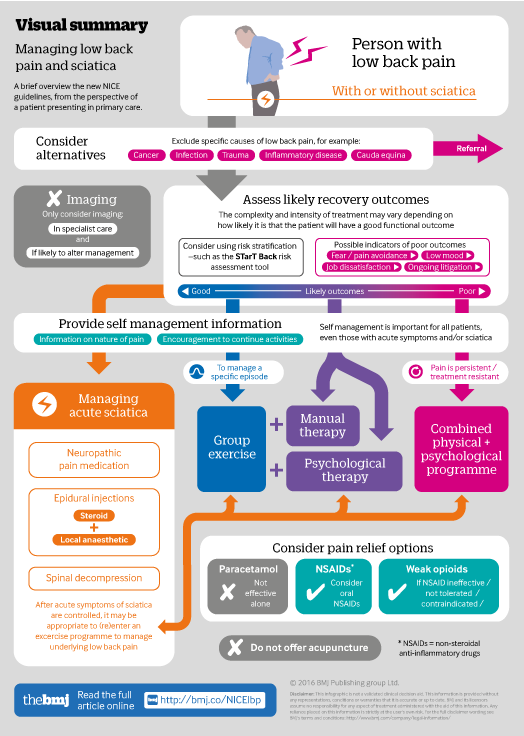
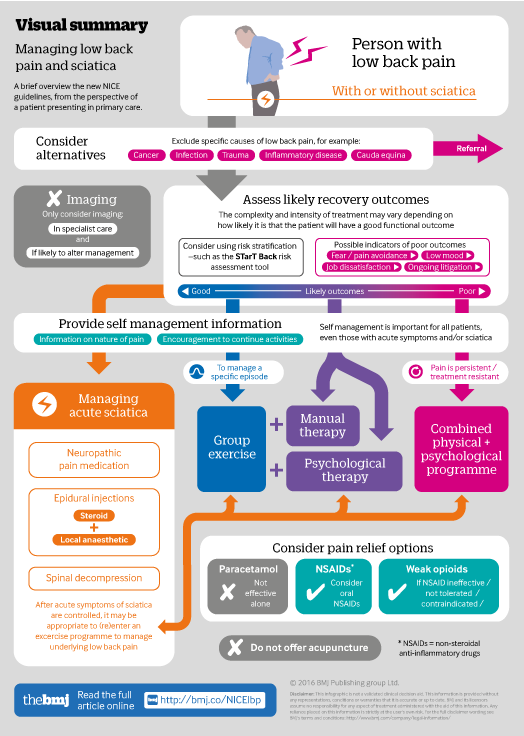
Infographic available
Click here for a visual overview of assessment and management for those with low back pain and/or sciatica.
Rapid Response:
Author's reply re: Low back pain and sciatica: summary of NICE guidance
We thank the rapid responders for the feedback on our summary.[1] The infographic[2] was designed from the perspective of a patient presenting in primary care, and the article focussed on 19 of the 41 recommendations in the guideline[3], as encapsulated in the ‘What you need to know’ box.
With respect to Andrew Frank’s comments:
We agree that that management needs to be personalised. The NICE guideline states: "…the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian…"[3]. Our summary states that clinicians should consider using risk stratification “to inform shared decision-making about stratified management.”
The Guideline Development Group (GDG) found no evidence to support the comment "…suggesting that X-Rays can confirm the spine’s suitability for exercise therapy..." Most of the evidence in favour of imaging reviewed by the GDG was obtained from a single RCT performed in a secondary setting of care, and was contrary to the evidence from several large cohort studies.[4] The GDG considered imaging was unlikely to be cost effective in a primary care setting, whilst it could be cost effective in those cases where imaging in specialist settings of care could lead to a change in management.[4]
We agree that ‘remaining in work’ and ‘return to work’ are important outcomes. Our summary mentioned the time lost from work, and the proportion of people who never return to work following an episode of LBP. A systematic review of return to work programmes was included in the full guideline, and stated that there was a "lack of evidence for a specific intervention or programme that could be recommended to enable people to return to work.”[4] The GDG discussed the “broader evidence highlighting [the] benefits of enabling people to return to work or their usual activities…” and agreed a consensus statement that an outcome of the management recommendations in the guideline was to enable people to return to work or their usual activities.[4]
With regards the definition of sciatica, this is defined in the NICE guideline as "leg pain secondary to lumbosacral nerve root pathology”.[3] The guideline explains that “sciatica is a term that patients and clinicians understand, and is widely used in the literature to describe neuropathic leg pain secondary to compressive spinal pathology.”[3] We agree that referred pain in the leg is an important differential and that the approach to management will be different if there is nerve root pathology or dural irritation. Throughout the guideline the GDG considered interventions and outcomes for people with sciatica separately from those with referred pain where the investigators were able to make that differentiation, and this is reflected in the acute sciatica pathway in the BMJ infographic accompanying this article.[2] However, in many studies, the investigators could not rigorously make that differentiation, and the GDG included these studies in the 'low back pain with or without sciatica' population in the pre-specified population groupings for each systematic review.[4] Although diagnostic accuracy reviews have been published, the GDG did not find any evidence for clinical examination tests that would both reliably diagnose sciatica AND lead to specific treatments that would improve patient outcomes (test and treat studies). [4] Therefore, the issue of referred pain versus neuropathic or nerve root pain remains a clinical management issue that was not resolved by the reviews undertaken by the GDG, and hence no recommendations were made in this regard.[4]
References
1. Bernstein IA, Malik Q, Carville S, Ward S. Low back pain and sciatica: summary of NICE guidance. BMJ 2017:i6748. http://dx.doi.org/10.1136/bmj.i6748
2. Bernstein IA, Malik Q, Carville S, Ward S. Low back pain and sciatica: summary of NICE guidance; Visual summary. BMJ 2017:i6748. http://www.bmj.com/content/bmj/suppl/2017/01/06/bmj.i6748.DC1/beri151216...
3. National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management (NICE Guideline NG59). 2016. www.nice.org.uk/guidance/ng59
4. National Guideline Centre, Royal College of Physicians. Low back pain and sciatica in over 16s: assessment and management—full guideline. National Institute for Health and Care Excellence, 2016. www.nice.org.uk/guidance/ng59/evidence
Competing interests: We declare the following interests based on NICE's policy on conflicts of interests (www.nice.org.uk/Media/Default/About/Who-we-are/Policies-and-procedures/code-of-practice-for-declaring-and-managing-conflicts-of-interest.pdf). The authors’ full statements are available online (www.nice.org.uk/guidance/NG59/documents/committee-member-list). IB is employed by London North West Healthcare NHS Trust, is a partner at Gordon House Surgery, and is employed by NHS Ealing CCG as clinical commissioning lead for MSk services, London; he received funding, travel, and subsistence allowances for committee work, lecturing, and organising educational workshops from NHS Ealing CCG, the Association for Medical Osteopathy, the Arthritis and Musculoskeletal Alliance, the NHS Alliance, the British Institute of Musculoskeletal Medicine, the British Society for Rheumatology, CloserStill Media Healthcare, Royal College of General Practitioners, Imperial College London, and NICE. SC is employed by the Royal College of Physicians, London. SW is employed by Brighton and Sussex University Hospitals NHS Trust, Brighton. He was a director of Back@Work until January 2016; a company that provides a community pain management service for the residents of mid-Sussex. He received accommodation, travel, and subsistence allowances for committee work and lecturing from the American Society of Interventional Pain Physicians and NICE. He has lectured or provided expert opinion (non-remunerated) at meetings at the Faculty of Pain Medicine, St Thomas’ Hospital, the Congress of the European Pain Federation, and the Spinal Intervention Society.