Abstract
To measure high-sensitivity C-reactive protein (hsCRP) levels and to assess the presence of metabolic syndrome (MS) after puerperium in women diagnosed with various hypertensive disorders during pregnancy (HDP), a consecutive, cross-sectional case study at the 15th week after gestation. The sample consisted of 264 women who were admitted to a women's hospital. The diagnoses consisted of transient gestational hypertension (TGH=43.2%), preeclampsia (PC=29.5%), chronic hypertension (CH=20.1%) and PC superimposed on CH (7.2%). A diagnosis of previous hypertension was present in 45.8% of the CH group. The prevalence of MS was 16.7% (CH=42.1%, TGH=13.9%, PC=4.1%, P<0.001). The average hsCRP levels for the CH, TGH and PC groups were 3.79±2.76, 3.55±3.15 and 2.89±3.02, respectively (P=0.040). The levels of hsCRP were higher in women with MS (4.71±3.15 vs. 3.01±2.88 mg l−1 in those without MS, P<0.001), and they increased when a higher number of MS criteria was fulfilled (P<0.001). The results demonstrated a positive correlation between hsCRP levels and body mass index (BMI) (r=0.46), waist circumference (r=0.50) or the number of fulfilled MS criteria (r=0.56). The results suggest differences in vascular risk that depend on the type of HDP and on the prevalence of MS. The prevalence of MS was notably higher in the CH group, intermediate among the TGH group and much lower in the PC group. Differences in hsCRP levels also depended on the type of HDP (higher levels in CH and TGH patients in comparison with PC patients). Women with MS had higher hsCRP levels compared with women without MS, and the levels correlated with the number of MS criteria fulfilled. This result suggests that subclinical inflammatory status is correlated with the number of MS components present. Furthermore, hsCRP levels increased with increasing BMIs and waist circumferences.
Similar content being viewed by others
Introduction
Hypertension, the most common medical complication that occurs during gestation, is reported in 6–10% of all pregnancies.1 Its presence has been related to an increased risk of cardiovascular disease (CVD) in the future, although the mechanisms defining this association are not well established. Moreover, there is a lack of prospective longitudinal studies regarding how vascular dysfunction and the development of CVD could progress over time.1, 2, 3, 4, 5, 6, 7 Thus, different reports have related the preexisting hypertension in pregnancy to a higher risk of hypertension, coronary heart disease and cerebrovascular disease later in life, as well as an earlier onset of these diseases.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 Similarly, a higher prevalence of metabolic syndrome (MS) has been described to occur several years after gestation in women with prior preeclampsia (PC) or gestational hypertension in comparison with those with non-hypertensive pregnancies.16 This syndrome is considered to be an independent risk factor for future CVD.17 Increased plasma levels of high-sensitivity C-reactive protein (hsCRP) are considered to be inflammatory and vascular risk markers,18 and these levels have been found to be increased during PC and gestational hypertension.5 The cause for these augmented risks may be the long-term development of metabolic, inflammatory and vascular changes.
Hypertensive disorders during pregnancy (HDP) are classified into different types depending on the time of onset, their persistence beyond 12 weeks after childbirth and proteinuria:1 chronic hypertension (CH), preeclampsia (PC), transient gestational hypertension (TGH) and preeclampsia superimposed on chronic hypertension (PC/CH). An accurate diagnosis of the type of HDP requires evaluation of the patient for at least 12 weeks after the end of gestation to confirm the persistence or disappearance of raised blood pressure (BP) levels. These different types of HDP may have distinct underlying pathogenic mechanisms and implications in the future development of CVD. While an elevated BP is the main physio-pathological characteristic of CH, elevated BP in PC is important to note as a sign of a multisystemic underlying disorder.1, 5
The presence of HDP may help to identify a group of women with an increased vascular risk and a predisposition to develop cardiovascular events; this risk could be different depending on the type of HDP. The aim of our study was to evaluate the different clinical and biological vascular risk parameters in the post gestational medical appointment (at 15 weeks after delivery), to evaluate the prevalence of MS and its relation to hsCRP as an indicator of vascular risk and to investigate possible differences in these parameters and vascular risk depending on the presented form of HDP.
Methods
This was a cross-sectional study of post gestational women 15 weeks after delivery. The study population consisted of all pregnant women diagnosed with hypertension and admitted to a women's hospital (Virgen del Rocío University Hospital, Seville, Spain) for any cause, including a healthy labor and delivery, within 16 consecutive months (2005–2007). The diagnosis of hypertension was made on the basis of repeated systolic BP readings of ⩾140 mm Hg and/or diastolic readings of ⩾90 mm Hg.1 All patients were reviewed at 15 weeks after delivery and were classified according to the accepted criteria of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy1 into the following groups: (1) CH, which is defined as hypertension present before pregnancy or diagnosed before the 20th week of gestation, as well as cases of hypertension diagnosed for the first time during pregnancy that do not resolve postpartum and persist longer than 12 weeks after delivery; (2) PC, which is defined as development of hypertension after 20 weeks of gestation accompanied by proteinuria of ⩾300 mg in 24 h that are resolved after gestation; (3) TGH, that displays a similar time of onset as PC, but is not marked by proteinuria and is resolved within 3 months following delivery; and (4) PC/CH, that is diagnosed when criteria for both entities are simultaneously present in the same patient.
The persistence of hypertension at 15 weeks postpartum was assessed by self-measurements (at home) of BP carried out by the patient with validated devices and by measurements obtained in the office by a trained nurse with a mercury sphygmomanometer. In both cases, technical measurements of BP were acquired according to the recommendations of the European Society of Hypertension.4 When doubts or contradictory data existed, BP monitoring over a 24-h period was carried out to correctly classify the patients into their specific class of HDP. The limits considered for the diagnosis of hypertension were proposed by the guidelines of the European Societies of Hypertension and Cardiology in 2007:4 ⩾140 and/or 90 mm Hg for clinical measurements, ⩾135/85 for home measurements and ⩾130/80 for 24-h average measurements (135/85 during activity and 120/70 at night). Meanwhile, we considered women who were under antihypertensive treatment to be hypertensive subjects independent of measured BP levels. We only used clinical measurements to compare BP levels among the four groups of HDP.
We used the following exclusion criteria: secondary hypertension, preexisting diabetes mellitus or dyslipidemia, or the development of gestational diabetes during pregnancy. These standards were met to provide a more accurate evaluation of the vascular risk specifically attributed to BP elevation.
In each case, at 15-week postpartum evaluation, information was recorded with regard to patient characteristics and obstetric features, and the body mass index (BMI) was calculated to evaluate obesity levels. With regard to the presence of hypertension in other family members, we only considered first-degree relatives. In relation to the subjects’ smoking status, an ex-smoker was defined as one who had abstained from smoking for at least 1 full year. A biochemical blood test (following fasting for 12 h) was performed to test levels of the following: glycated hemoglobin (HbA1c) (measured by the high performance liquid chromatography (HPLC) method), glycemia (enzymatic spectrophotometry with glucose oxidase), total cholesterol (enzymatic spectrophotometry), low- (LDL) and high-density lipoprotein (HDL) levels (LDL via the Friedewald formula and HDL via enzymatic spectrophotometry), triglycerides (enzymatic spectrophotometry), apolipoproteins A1 and B (immunonephelometry), uric acid (enzymatic spectrophotometry with uricase), hsCRP (immunonephelometry) and homocysteine concentrations (HPLC). A diagnosis of MS was determined according to the National Cholesterol Education Program—Adult Treatment Panel III (NCEP–ATP III) criteria19 (MS criteria included at least three of the following: waist circumference >88 cm, triglycerides ⩾150 mg dl−1, HDL <50 mg dl−1, BP ⩾130 and/or ⩾85 mm Hg and/or fasting glucose ⩾110 mg dl−1).
A statistical analysis was performed using the Statistical Package for the Social Sciences software (SPSS, IBM Company). Data were expressed as the mean ± s.d. for quantitative parameters and as a percentage of the total for qualitative parameters. A statistically significant difference among data was defined using a P-value of <0.05. First, we carried out a descriptive study of the characteristics of each group. We then performed comparisons among the groups. In order to compare continuous parameters, an ANOVA was used when samples were normal, which was followed by a Bonferroni test for post-hoc analysis when appropriate. For the groups with samples that were not normal, Kruskal–Wallis and Mann–Whitney's U tests were used. A χ2-test was used to compare the categorical parameters. Finally, we analyzed the association among different variables by means of bivariate correlation and linear regression.
Results
In total, 264 pregnant women were included in this study. The general characteristics of these subjects and comparisons among groups appear in Tables 1,2,3. In the CH group and the PC/CH group, 38.8 and 31.6% of women had a history of smoking (during the time of the study or in the past), respectively. Lower percentages were identified in cases of TGH (28.3%) and PC (24.4%), although no statistical differences were found among the groups. The prevalence of known hypertension before pregnancy was 52.8% in the case of the CH group and 26.3% in the PC/CH group. When we considered all women with CH (with or without superimposed PC), the prevalence of pregestational hypertension was 45.8%.
The presence of isolated PC was associated with lower BMI and lower waist circumference, with the results being statistically significantly different when we compared the PC with the CH or the TGH groups (P⩽0.001). No statistically significant differences were found among the lipid profiles (except for levels of triglycerides), including rates among cholesterol parameters (total cholesterol/HDL, LDL/HDL), apolipoproteins A1 and B, fasting glucose, HbA1c, uric acid and homocysteine. HsCRP levels were different depending on the presented HDP; levels were significantly higher in women with CH than in those in the PC group. The TGH patients also had higher hsCRP levels than the PC group, with a P value near the level of significance (P=0.052).
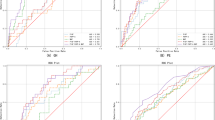
The prevalence of MS, according to ATP III criteria, was higher in cases of the CH patients, followed by TGH patients. The lowest prevalence of MS was found in preeclamptic women, with significant differences among the groups (Figure 1). Sufficient criteria to fulfill a diagnosis of MS were absent in 83.3% of the patients. In patients with MS, hsCRP levels were higher than those in the group without MS. The hsCRP levels in MS patients (16.7%) were 4.71±3.15 mg l−1 and were 3.01±2.88mg l−1 in patients without MS (83.3%, P<0.001). We also studied the number of criteria (of the maximum of five) fulfilled by the patients (with or without MS), and its relation to hsCRP levels (Table 4). Most women (61.3%) presented at least one or two of these criteria. The hsCRP levels were increased as a greater number of criteria were satisfied (Figure 2). Because of the small number of women in which all five criteria were presented, subjects presenting with four and five criteria were combined and considered to be a unique group for statistical analysis.
Results from analyses using bivariate correlation and a linear regression model demonstrated that hsCRP levels were positively correlated with the number of fulfilled criteria for MS (r=0.36, <0.001), BMI (r=0.46, P<0.001) and waist circumference (r=0.50, P<0.001) (Figure 3). The association between the BMI and the number of components of MS was also significant (r=0.56, P<0.001). The parameters that were used for the regression analyses were age, smoking status, BP (systolic and diastolic), lipid profile, fasting glucose, BMI, waist circumference and number of components of MS.
Discussion
On the basis of widely accepted criteria,1 an accurate diagnosis of hypertension presented during gestation demands an evaluation at least 12 weeks after delivery to determine whether increased BP levels persist. In our study, an evaluation was carried out at 15 weeks; therefore, we retrospectively established the exact diagnosis of the hypertensive disorder present during pregnancy. Furthermore, the various measurements were determined in a basal state, and thus were not under the influence of gestation. The presence of hypertension during gestation presents an opportunity to identify women with constitutional hypertension, which was not previously diagnosed in this group of patients. An important finding of our study was the high percentage of women who remain hypertensive after pregnancy, in whom the gestation constitutes the time of such a diagnosis; therefore, more than half of the women with CH (54.2%) were not known to be hypertensive before the current gestation. Therefore, post gestational evaluation is both necessary and important in identifying this subgroup of patients, who may subsequently undergo a follow-up examination; and continued evidence of hypertension may further the need for intensive preventative measures and pharmacological treatment.
BP levels were the highest (in the range of hypertension) among women with CH; however, these levels may be lower than expected as many patients in this group were under antihypertensive treatment because of the persistence of raised BP at 15 weeks postpartum. Women with TGH showed BP levels (both systolic and diastolic) significantly higher than the PC group. Interestingly, women with TGH were in the range of prehypertension,20 and this finding may indicate the possibility of a higher future risk of developing hypertension or target organ disease in patients with TGH. It may even indicate the possibility of an earlier onset of hypertension or target organ disease. Nevertheless, this hypothesis cannot be proven by the information currently available from long-term studies. Both PC and TGH have been related to a higher risk of hypertension in the later years of life,5, 16 but data regarding which of these groups has a higher risk are debatable and controversial.6, 11, 12
Various metabolic changes are normally observed in a routine pregnancy, including hyperlipidemia (for example, increased triglycerides or small-density LDL particles and decreased HDL), or a hypercoagulability and proinflammatory state. Similarly, there is a progressive increase in insulin resistance and hyperinsulinism until the third trimester (to facilitate the transfer of glucose to the fetus), which returns to normal values postpartum.5, 21, 22, 23, 24 Insulin resistance is considered to be a key pathogenic factor in the development of MS,18, 25 and this syndrome constitutes an independent risk factor for CVD.17 Girouard et al.24 found that women who had PC or TGH at a mean of 7.8 years before the time of the study showed a higher insulin resistance, according to the HOMA index, than other subjects with normotensive pregnancies. These women also demonstrated a greater rate of obesity (measured by BMI and waist circumference) and other metabolic disorders (hydrocarbonate intolerance and dyslipidemia), higher hsCRP levels and interleukin-6 as inflammatory markers, and a higher prevalence of hypertension. The same authors previously reported an augmented risk (up to three- or fourfold) of developing MS (ATP III criteria) after a hypertensive pregnancy in comparison with the control group, and the risk was higher in cases of TGH (fourfold increase) than in cases of PC (two- to fourfold increase).16 Our findings related to MS prevalence are in agreement with this data, and they suggest that this augmented risk could already be present early after gestation. Changes demonstrated in normal pregnancy, which are similar to those described as vascular risk factors in the general population, may be emphasized in cases of HDP and have a role in the increased risk of future CVD observed in these patients. In this respect, an increase in insulin resistance, obesity, endothelial dysfunction, dyslipidemia, hydrocarbonate intolerance or inflammatory markers has been described during pregnancy in cases of PC.2, 16, 21, 23, 26 Although fewer cases have been reported, TGH has also demonstrated an association with insulin resistance.23, 26 Some authors even consider the presence of hypertension or other complications during pregnancy to indicate patients predisposed to a higher vascular risk in the future.22 In our study, an examination of the immediate postpartum period revealed no differences in hydrocarbonate or lipid profiles with the exception of triglycerides. This finding may result from the fact that a longer follow-up period is necessary to reveal this disorder. Nevertheless, we found that patients with CH and TGH presented a higher rate of obesity, as assessed by BMI, 15 weeks after delivery in comparison with cases of PC. The CH and TGH cases demonstrated a predominantly central or abdominal obesity (measured by waist circumference) that is known to pose a higher cardiovascular risk.19 Anyway, the obesity in the cases of CH and TGH may have been present before the current gestation and may have been a pre-pregnancy condition,24, 27 which suggests a predisposition to MS unrelated to pregnancy. The prevalence of MS was considerably higher in cases of CH (33–42%) than in TGH cases (14%, likewise a raised prevalence) and the prevalence was low in cases of PC (only 4%). The varying rates of MS associated with each type of HDP may indicate itself that different vascular risks exist among the types of HDP during the time of the study and probably into the long-term. Data from linear regression analyses are in agreement with previously reported information and suggest that MS and insulin resistance are related to higher hsCRP levels because both are closely related to obesity (measured by BMI) and central adiposity (assessed by waist circumference). This association has been previously reported, suggesting that hsCRP is a marker for MS and endothelial dysfunction, and is related to insulin resistance.28
The observed difference in hsCRP levels and the association between increased hsCRP levels and the presence of MS were remarkable findings in our study. To the best of our knowledge, there have been no previous studies on this subject focusing on this group of patients. The significantly greater hsCRP levels in the CH patients and the nearly significant findings in TGH (P=0.052) in comparison with PC may indicate a basal subclinical inflammatory status in the first groups, which acts as a risk marker and may be related to the different prevalence of MS found in this study. In this respect, many studies have shown the importance of hsCRP as an indicator of CVD risk and as a predictor for the development of CVD.28, 29 Recently, proatherogenic properties have been attributed to hsCRP, so it may have a causal role in addition to being a marker in the development of atherosclerosis.18 In this way, patients with hsCRP concentrations less than 1 mg l−1 are considered to be at low risk of developing CVD, whereas concentrations greater than 3 mg l−1 indicate a high risk and concentrations between 1 and 3 mg l−1 indicate a medium risk.28 Recently, the JUPITER study has supported the importance of hsCRP as a predictor for developing cardiovascular events.30 In addition, women who had MS showed higher hsCRP levels that correlated with the number of fulfilled criteria for the syndrome, which suggests that subclinical inflammatory status increases when more components of MS are present. The association of MS and hsCRP has been previously reported, but we have not found published data relating hsCRP levels to the number of criteria for MS. In accordance with previous results, hsCRP levels were similarly correlated with a greater BMI and waist circumference.
To our knowledge, there are no studies comparing the four possible types of HDP and no studies that evaluate the early vascular risk in a post-gestational evaluation. In accordance with our results, women with hypertension (as opposed to PC) may have a higher vascular risk because they have a greater incidence of smoking and a family history of hypertension, high BP, high BMI and prevalence of MS. These factors may explain the higher hsCRP levels (as an inflammatory marker) that we have found in these patients. The PC/CH group showed features of both CH and PC.
Our study also supports the theory that there is a varying risk of developing hypertension or CVD later in life that depends on the type of hypertension suffered during pregnancy. Nevertheless, more long-term and follow-up studies are needed to confirm these hypotheses and to understand the full impact of HDP with regard to future vascular risk. Finally, our results highlight the necessity of a post gestational evaluation at a minimum of 12 weeks after labor (in a basal status) to establish the exact diagnosis of HDP and to ensure the proper evaluation of vascular risk. By doing so, one can take primary preventative measures and promote lifestyle changes and can identify those women who remain hypertensive and that require pharmacological treatment, follow-up and more intensive preventive measures.
References
Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol 2000; 183: S1–S22.
Sibai B, Dekker G, Kupferminc M . Pre-eclampsia. Lancet 2005; 365: 789–799.
Banerjee M, Cruickshank JK . Pregnancy as the prodrome to vascular dysfunction and cardiovascular risk. Nat Clin Prac Cardiovasc Med 2006; 3: 596–603.
Guidelines for the Management of Arterial Hypertension. The task force for the management of arterial hypertension of the European society of hypertension and of the European society of cardiology. J Hypertens 2007; 25: 1105–1187.
Garovic VD, Hayman SR . Hypertension in pregnancy: an emerging risk factor for cardiovascular disease. Nat Clin Prac Nephrol 2007; 3: 613–622.
Bellamy L, Casas JP, Hingorani AD, Williams DJ . Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 2007; 335: 974–977.
Harskamp RE, Zeeman G . Preeclampsia: at risk for remote cardiovascular disease. Am J Med Sci 2007; 334: 291–295.
Rodie VA, Freeman DJ, Sattar N, Greer IA . Pre-eclampsia and cardiovascular disease: metabolic syndrome of pregnancy? Atherosclerosis 2004; 175: 189–202.
Smith GC, Pell JP, Walsh D . Pregnancy complications and maternal risk of ischaemic heart disease: a retrospective cohort study of 129290 births. Lancet 2001; 357: 2002–2006.
Irgens HU, Reisaeter L, Irgens LM, Lie RT . Long term mortality of mothers and fathers after pre-eclampsia: population based cohort study. BMJ 2001; 323: 1213–1217.
Marín R, Gorostidi M, Portal CG, Sánchez M, Sánchez E, Álvarez J . Long-term prognosis of hypertension in pregnancy. Hypertens Pregnancy 2000; 19: 199–209.
Wilson BJ, Watson MS, Prescott GJ, Sunderland S, Campbell DM, Hannaford P, Smith WCS . Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: results from cohort study. BMJ 2003; 326: 845–849.
Jonsdottir LS, Arngrimsson R, Geirsson RT, Sigvaldason H, Sigfusson N . Death rates from ischemic heart disease in women with a history of hypertension in pregnancy. Acta Obstet Gynecol Scand 1995; 74: 772–776.
Hannaford P, Ferry S, Hirsch S . Cardiovascular sequelae of toxaemia of pregnancy. Heart 1997; 77: 154–158.
Kestenbaum B, Selifer SL, Easterling TR, Gillen DL, Critchlow CW, Stehman-Breen CO, Schwartz SM . Cardiovascular and thromboembolic events following hypertensive pregnancy. Am J Kidney Dis 2003; 42: 982–989.
Forest JC, Girouard J, Mass J, Moutquin JM, Kharfi A, Ness RB, Roberts JM, Giguère Y . Early occurrence of metabolic syndrome after hypertension in pregnancy. Obstet Gynecol 2005; 105: 1373–1380.
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, Taskinen MR, Groop L . Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001; 24: 683–689.
Jialal I, Devaraj S, Venugopal SK . C-Reactive Protein: risk marker or mediator in atherothrombosis? Hypertension 2004; 44: 6–11.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001; 285: 2486–2497.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ, and the National High Blood Pressure Education Program Coordinating Committee. The seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood Pressure. JAMA 2003; 289: 2560–2572.
Seely EW, Solomon CG . Insulin resistance and its potential role in pregnancy-induced hypertension. J Clin Endocrinol Metab 2003; 88: 2393–2398.
Williams D . Pregnancy: a stress test for life. Curr Opin Obstet Gynecol 2003; 15: 465–471.
Solomon CG, Seely EW . Hypertension in pregnancy. A manifestation of the insulin resistance syndrome? Hypertension 2001; 37: 232–239.
Girouard J, Giguère Y, Moutquin JM, Forest JC . Previous hypertensive disease of pregnancy is associated with alterations of markers of insulin resistance. Hypertension 2007; 49: 1056–1062.
Alberti KG, Zimmet PZ . Definition, diagnosis and classification of diabetes mellitus and its complication. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998; 15: 539–553.
Pouta A, Hartikainen AL, Sovio U, Gissler M, Laitinen J, McCarthy MI, Ruokonen A, Elliott P, Järvelin MR . Manifestation of metabolic syndrome after hypertensive pregnancy. Hypertension 2004; 43: 825–831.
Barden AE, Beilin LJ, Ritchie J, Walters BN, Michael C . Does a predisposition to the metabolic syndrome sensitize women to develop preeclampsia? J Hypertens 1999; 17: 1307–1315.
Poledne R, Lorenzova A, Stávek P, Valenta Z, Hubácek J, Suchánek P, Pitha J . Proinflammatory statusm, genetics and atherosclerosis. Physiol Res 2009; 58: S111–S118.
Ridker PM, Cushman M, Stampferd MJ, Tracy RP, Hennekens CH . Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 1997; 336: 973–979.
Ridker PM, Danielson E, Fonseca FAH, Genest J, Gotto AM, Kastelein JJP, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ . Rosuvastatin to prevent vascular events in men and women with elevated C-Reactive Protein. N Engl J Med 2008; 359: 2195–2207.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Vallejo Vaz, A., Guisado, M., García-Junco, P. et al. Differences in the prevalence of metabolic syndrome and levels of C-reactive protein after puerperium in women with hypertensive disorders during pregnancy. Hypertens Res 33, 1012–1017 (2010). https://doi.org/10.1038/hr.2010.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.131
Keywords
This article is cited by
-
Study protocol for the sheMATTERS study (iMproving cArdiovascular healTh in new moThERS): a randomized behavioral trial assessing the effect of a self-efficacy enhancing breastfeeding intervention on postpartum blood pressure and breastfeeding continuation in women with hypertensive disorders of pregnancy
BMC Pregnancy and Childbirth (2023)