Abstract
Introduction and hypothesis
To review the safety and efficacy of uterine preservation surgery.
Methods
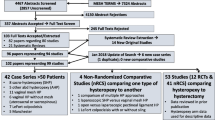
Every four years and as part of the Fifth International Collaboration on Incontinence we reviewed the English-language scientific literature after searching PubMed, Medline, Cochrane library and Cochrane database of systematic reviews, published up to January 2012. Publications were classified as level 1 evidence (randomised controlled trials [RCT] or systematic reviews), level 2 (poor quality RCT, prospective cohort studies), level 3 (case series or retrospective studies) and level 4 case reports. The highest level of evidence was utilised by the committee to make evidence-based recommendations based upon the Oxford grading system. Grade A recommendation usually depends on consistent level 1 evidence. Grade B recommendation usually depends on consistent level 2 and/or 3 studies, or “majority evidence” from RCTs. Grade C recommendation usually depends on level 4 studies or “majority evidence” from level 2/3 studies or Delphi processed expert opinion. Grade D “no recommendation possible” would be used where the evidence is inadequate or conflicting and when expert opinion is delivered without a formal analytical process, such as by Delphi.
Results
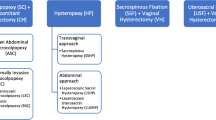
A wide variety of surgical options remain for women presenting with uterine prolapse without contraindications to uterine preservation. However, long-term data are limited and the need for subsequent hysterectomy unknown (grade C). Sacrospinous hysteropexy is as effective as vaginal hysterectomy and repair in retrospective comparative studies and in a meta-analysis with reduced operating time, blood loss and recovery time. However, in a single RCT there was a higher recurrence rate associated with sacrospinous hysteropexy compared with vaginal hysterectomy (grade D). Severe prolapse increases the risk of recurrent prolapse after sacrospinous hysteropexy. In consistent level 2 evidence sacrospinous hysteropexy with mesh augmentation of the anterior compartment was as effective as hysterectomy and mesh augmentation with no significant difference in the rate of mesh exposure between the groups (grade B). Level 1 evidence from a single RCT suggests that vaginal hysterectomy and uterosacral suspension were superior to sacral hysteropexy based on reoperation rates, despite similar anatomical and symptomatic improvement (grade C). Consistent level 2 and 3 evidence suggests that sacral hysteropexy (open or laparoscopic) was as effective as sacral colpopexy and hysterectomy in anatomical outcomes; however, the sacral colpopexy and hysterectomy were associated with a five times higher rate of mesh exposure compared with sacral hysteropexy (grade B). Performing hysterectomy at sacral colpopexy was associated with a four times higher risk of mesh exposure compared with sacral colpopexy without hysterectomy (grade B).
Conclusion
While uterine preservation is a viable option for the surgical management of uterine prolapse the evidence on safety and efficacy is currently lacking.
Similar content being viewed by others
References
Frick AC, Walters MD, Larkin KS, Barber MD (2010) Risk of unanticipated abnormal gynecologic pathology at the time of hysterectomy for uterovaginal prolapse. Am J Obstet Gynecol 202(5):507e1–507e4
Ayhan A, Esin S, Guven S, Salman C, Ozyuncu O (2006) The Manchester operation for uterine prolapse. Int J Gynaecol Obstet 92(3):228–233
Thomas AG, Brodman ML, Dottino PR, Bodian C, Friedman F Jr, Bogursky E (1995) Manchester procedure vs. vaginal hysterectomy for uterine prolapse. A comparison. J Reprod Med 40(4):299–304
Tipton RH, Atkin PF (1970) Uterine disease after the Manchester repair operation. J Obstet Gynaecol Br Commonw 77(9):852–853
Williams BF (1966) Surgical treatment for uterine prolapse in young women. Am J Obstet Gynecol 95(7):967–971
de Boer TA, Milani AL, Kluivers KB, Withagen MI, Vierhout ME (2009) The effectiveness of surgical correction of uterine prolapse: cervical amputation with uterosacral ligament plication (modified Manchester) versus vaginal hysterectomy with high uterosacral ligament plication. Int Urogynecol J Pelvic Floor Dysfunct 20(11):1313–1319
Kalogirou D, Antoniou G, Karakitsos P, Kalogirou O (1996) Comparison of surgical and postoperative complications of vaginal hysterectomy and Manchester procedure. Eur J Gynaecol Oncol 17(4):278–280
Thys SD, Coolen A, Martens IR et al (2011) A comparison of long-term outcome between Manchester Fothergill and vaginal hysterectomy as treatment for uterine descent. Int Urogynecol J 22(9):1171–1178
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE (2010) One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J 21(2):209–216
Jeng CJ, Yang YC, Tzeng CR, Shen J, Wang LR (2005) Sexual functioning after vaginal hysterectomy or transvaginal sacrospinous uterine suspension for uterine prolapse: a comparison. J Reprod Med 50(9):669–674
Dietz V, de Jong J, Huisman M, Schraffordt Koops S, Heintz P, van der Vaart H (2007) The effectiveness of the sacrospinous hysteropexy for the primary treatment of uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 18(11):1271–1276
Dietz V, Huisman M, de Jong JM, Heintz PM, van der Vaart CH (2008) Functional outcome after sacrospinous hysteropexy for uterine descensus. Int Urogynecol J Pelvic Floor Dysfunct 19(6):747–752
Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E (2003) Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol 188(3):645–650
Hefni MA, El-Toukhy TA (2006) Long-term outcome of vaginal sacrospinous colpopexy for marked uterovaginal and vault prolapse. Eur J Obstet Gynecol Reprod Biol 127(2):257–263
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P (2001) Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct 12(6):381–384
Van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH (2003) Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct 14(5):350–355; discussion 5
Lin TY, Su TH, Wang YL et al (2005) Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc 104(4):249–253
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE (2010) One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct 21(2):209–216
Hefni MA, El-Toukhy TA (2006) Long-term outcome of vaginal sacrospinous colpopexy for marked uterovaginal and vault prolapse. Eur J Obstet Gynecol Reprod Biol 127(2):257–263
Kovac SR, Cruikshank SH (1993) Successful pregnancies and vaginal deliveries after sacrospinous uterosacral fixation in five of nineteen patients. Am J Obstet Gynecol 168(6 Pt 1):1778–1783; discussion 83–86
Richardson DA, Scotti RJ, Ostergard DR (1989) Surgical management of uterine prolapse in young women. J Reprod Med 34:388–392
Paraiso MF, Ballard LA, Walters MD, Lee JC, Mitchinson AR (1996) Pelvic support defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. Am J Obstet Gynecol 175(6):1423–1430
Maher C, Feiner B, Baessler K, Adams EJ, Hagen S, Glazener CM (2010) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014
Feiner B, Gietelink L, Maher C (2010) Anterior vaginal mesh sacrospinous hysteropexy and posterior fascial plication for anterior compartment dominated uterovaginal prolapse. Int Urogynecol J 21(2):203–208
Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2006) Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct 17(4):315–320
McDermott CD, Terry CL, Woodman PJ, Hale DS (2011) Surgical outcomes following total Prolift: colpopexy versus hysteropexy. Aust N Z J Obstet Gynaecol 51(1):61–66
Chu LC, Chuang FC, Kung FT, Huang KH (2012) Comparison of short-term outcomes following pelvic reconstruction with Perigee and Apogee systems: hysterectomy or not? Int Urogynecol J 23(1):79–84
Neuman M, Lavy Y (2007) Conservation of the prolapsed uterus is a valid option: medium term results of a prospective comparative study with the posterior intravaginal slingoplasty operation. Int Urogynecol J Pelvic Floor Dysfunct 18(8):889–893
Huang KH, Chuang FC, Fu HC, Kung FT. Polypropylene mesh as an alternative option for uterine preservation in pelvic reconstruction in patients with uterine prolapse. J Obstet Gynaecol Res 38(1):97–101
Inoue H, Sekiguchi Y, Kohata Y et al (2009) Tissue fixation system (TFS) to repair uterovaginal prolapse with uterine preservation: a preliminary report on perioperative complications and safety. J Obstet Gynaecol Res 35(2):346–353
Nicita G, Li Marzi V, Filocamo MT et al (2005) Uterus-sparing vaginal surgery of genitourinary prolapse employing biocompatible material. Urol Int 75(4):314–318
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)–a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct 18(7):743–752
Feiner B, Gietelink L, Maher C (2010) Anterior vaginal mesh sacrospinous hysteropexy and posterior fascial plication for anterior compartment dominated uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 21(2):203–208
Giles AE (1930) The effect of hysteropexy upon a subsequent pregnancy, and of pregnancy upon a previous hysteropexy. Proc R Soc Med 23(8):1170–1177
Swain J (1897) A case of ovarian cystoma associated with prolapsus uteri, treated by ovariotomy and hysteropexy. Br Med J 2(1911):399–400
Joshi VM (1993) A new technique of uterine suspension to pectineal ligaments in the management of uterovaginal prolapse. Obstet Gynecol 81(5 (Pt 1)):790–793
Nesbitt RE Jr (1989) Uterine preservation in the surgical management of genuine stress urinary incontinence associated with uterovaginal prolapse. Surg Gynecol Obstet 168(2):143–147
O’Brien PM, Ibrahim J (1994) Failure of laparoscopic uterine suspension to provide a lasting cure for uterovaginal prolapse. British journal of obstetrics and gynaecology 101(8):707–708
Chen G, Ling B, Li J et al (2010) Laparoscopic extraperitoneal uterine suspension to anterior abdominal wall bilaterally using synthetic mesh to treat uterovaginal prolapse. J Minim Invasive Gynecol 17(5):631–636
Arthure HG, Savage D (1957) Uterine prolapse and prolapse of the vaginal vault treated by sacral hysteropexy. J Obstet Gynaecol Br Emp 64(3):355–360
Stoesser FG (1955) Construction of a sacrocervical ligament for uterine suspension. Surg Gynecol Obstet 101(5):638–641
Addison WA, Timmons MC (1993) Abdominal approach to vaginal eversion. Clin Obstet Gynecol 36(4):995–1004
Van Lindert AC, Groenendijk AG, Scholten PC, Heintz AP (1993) Surgical support and suspension of genital prolapse, including preservation of the uterus, using the Gore-Tex soft tissue patch (a preliminary report). Eur J Obstet Gynecol Reprod Biol 50(2):133–139
Bai SW, Kim EH, Shin JS, Kim SK, Park KH, Lee DH (2005) A comparison of different pelvic reconstruction surgeries using mesh for pelvic organ prolapse patients. Yonsei Med J 46(1):112–118
Banu LF (1997) Synthetic sling for genital prolapse in young women. Int J Gynaecol Obstet 57(1):57–64
Barranger E, Fritel X, Pigne A (2003) Abdominal sacrohysteropexy in young women with uterovaginal prolapse: long-term follow-up. Am J Obstet Gynecol 189(5):1245–1250
Costantini E, Lazzeri M, Zucchi A, Bini V, Mearini L, Porena M (2011) Five-year outcome of uterus sparing surgery for pelvic organ prolapse repair: a single-center experience. Int Urogynecol J 22(3):287–292
Costantini E, Lombi R, Micheli C, Parziani S, Porena M (1998) Colposacropexy with Gore-tex mesh in marked vaginal and uterovaginal prolapse. Eur Urol 34(2):111–117
Costantini E, Mearini L, Bini V, Zucchi A, Mearini E, Porena M (2005) Uterus preservation in surgical correction of urogenital prolapse. Eur Urol 48(4):642–649
Demirci F, Ozdemir I, Somunkiran A, Doyran GD, Alhan A, Gul B (2006) Abdominal sacrohysteropexy in young women with uterovaginal prolapse: results of 20 cases. J Reprod Med 51(7):539–543
Jeon MJ, Jung HJ, Choi HJ, Kim SK, Bai SW (2008) Is hysterectomy or the use of graft necessary for the reconstructive surgery for uterine prolapse? Int Urogynecol J Pelvic Floor Dysfunct 19(3):351–355
Leron E, Stanton SL (2001) Sacrohysteropexy with synthetic mesh for the management of uterovaginal prolapse. BJOG 108(6):629–633
Roovers JP, van der Bom JG, van der Vaart CH, Schagen van Leeuwen JH, Heintz AP (2002) Abdominal versus vaginal approach for the management of genital prolapse and coexisting stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 13(4):224–231
Roovers JP, van der Vaart CH, van der Bom JG, van Leeuwen JH, Scholten PC, Heintz AP (2004) A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG 111(1):50–56
Costantini E, Lazzeri M, Bini V, Del Zingaro M, Zucchi A, Porena M (2011) Pelvic organ prolapse repair with and without prophylactic concomitant Burch colposuspension in continent women: a randomized, controlled trial with 8-year followup. J Urol 185(6):2236–2240
Price N, Slack A, Jackson SR (2011) Laparoscopic sacrocolpopexy: an observational study of functional and anatomical outcomes. Int Urogynecol J 22(1):77–82
Rosenblatt PL, Chelmow D, Ferzandi TR (2008) Laparoscopic sacrocervicopexy for the treatment of uterine prolapse: a retrospective case series report. J Minim Invasive Gynecol 15(3):268–272
Rosen DM, Shukla A, Cario GM, Carlton MA, Chou D (2008) Is hysterectomy necessary for laparoscopic pelvic floor repair? A prospective study. J Minim Invasive Gynecol 15(6):729–734
Diwan A, Rardin CR, Strohsnitter WC, Weld A, Rosenblatt P, Kohli N (2006) Laparoscopic uterosacral ligament uterine suspension compared with vaginal hysterectomy with vaginal vault suspension for uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 17(1):79–83
Maher CF, Carey MP, Murray CJ (2001) Laparoscopic suture hysteropexy for uterine prolapse. Obstet Gynecol 97(6):1010–1014
Medina C, Takacs P (2006) Laparoscopic uterosacral uterine suspension: a minimally invasive technique for treating pelvic organ prolapse. J Minim Invasive Gynecol 13(5):472–475
Krause HG, Goh JT, Sloane K, Higgs P, Carey MP (2006) Laparoscopic sacral suture hysteropexy for uterine prolapse. Int Urogynecol J Pelvic Floor Dysfunct 17(4):378–381
Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES (2011) Prevalence and risk factors for mesh erosion after laparoscopic-assisted sacrocolpopexy. Int Urogynecol J 22(2):205–212
Visco AG, Weidner AC, Barber MD et al(2001) Vaginal mesh erosion after abdominal sacral colpopexy. Am J Obstet Gynecol 184(3):297–302
Cundiff GW, Varner E, Visco AG et al (2008) Risk factors for mesh/suture erosion following sacral colpopexy. Am J Obstet Gynecol 199(6):688e1–688e5
Bensinger G, Lind L, Lesser M, Guess M, Winkler HA Abdominal sacral suspensions: analysis of complications using permanent mesh. Am J Obstet Gynecol 193(6):2094–2098
Brizzolara S, Pillai-Allen A (2003) Risk of mesh erosion with sacral colpopexy and concurrent hysterectomy. Obstet Gynecol 102(2):306–310
Culligan PJ, Murphy M, Blackwell L, Hammons G, Graham C, Heit MH (2002) Long-term success of abdominal sacral colpopexy using synthetic mesh. Am J Obstet Gynecol 187(6):1473–1480; discussion 81–82
Stepanian AA, Miklos JR, Moore RD, Mattox TF (2008) Risk of mesh extrusion and other mesh-related complications after laparoscopic sacral colpopexy with or without concurrent laparoscopic-assisted vaginal hysterectomy: experience of 402 patients. J Minim Invasive Gynecol 15(2):188–196
Acknowledgements
This publication results from the work of the Committee on Pelvic Organ Prolapse Surgery, part of the 5th International Consultation on Incontinence, held in Paris in February 2012, under the auspices of the International Consultation on Urological Diseases, and enabled by the support of the European Association of Urology.
The authors wish to acknowledge the fine work of previous consultations led by Professor Linda Brubaker.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of Committee 15 “Surgical Management of Pelvic Organ Prolapse” from the 5th International Consultation on Incontinence held in Paris, February 2012
This work has been previously published as: Maher C, Baessler K, Barber M, Cheon C, Deitz V, DeTayrac R, Gutman R, Karram M, Sentilhes L (2013) Surgical management of pelvic organ prolapse. In: Abrams, Cardozo, Khoury, Wein, (eds) 5th International Consultation on Incontinence. Health Publication Ltd, Paris, Chapter 15 and modified for publication in International Urogynaecology Journal.
Rights and permissions
About this article
Cite this article
Gutman, R., Maher, C. Uterine-preserving POP surgery. Int Urogynecol J 24, 1803–1813 (2013). https://doi.org/10.1007/s00192-013-2171-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2171-2