Abstract
Aims/hypothesis
The association between CHD and insulin sensitivity (Si) measured by the euglycaemic insulin clamp has not been examined previously. Earlier studies found a relationship between CHD and elevated plasma insulin, an analysis that may have been confounded by co-determination of proinsulin, which has evolved as a stronger predictor of CHD. The aim was to determine the longitudinal relationships between Si, intact proinsulin, 32–33 split proinsulin, specific insulin and subsequent CHD.
Methods
This was a population-based cohort study of 815 men in Uppsala, Sweden, aged 70 years at baseline with a follow-up of up to 10 years. Baseline insulin sensitivity was determined by euglycaemic insulin clamp. Fasting proinsulin, 32–33 split proinsulin and specific insulin concentrations were analysed using specific two-site immunometric assays. CHD was taken as diagnosed, if stated (in the event of death) on the Cause of Death Registry, or for subjects hospitalised for the first time with CHD, if CHD was recorded in the Hospital-Discharge Registry. The associations were analysed using Cox’s proportional hazards, presented as hazard ratios (HRs) with their 95% CIs for a one-SD increase in the predictor.
Results
In multivariate analysis, Si (HR:0.80, CI:0.65–0.97) adjusted for serum cholesterol, systolic blood pressure, fasting plasma glucose, BMI and smoking predicted CHD. Intact proinsulin (HR:1.18, CI:1.01–1.38), adjusted as the model above, predicted CHD, whereas 32–33 split proinsulin (HR:1.13, CI:0.95–1.35) or specific insulin (HR:1.07, CI:0.89–1.30) did not.
Conclusions/interpretation
Insulin resistance measured by the euglycaemic insulin clamp predicts subsequent CHD in elderly men. Proinsulin provides a better prediction of CHD than insulin.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus, hypertension and dyslipidaemia are associated with insulin resistance and an increased risk of CHD [1]. Atherosclerosis is associated with insulin resistance [2], but the extent to which insulin resistance contributes to the risk of subsequent CHD has so far mostly been studied by using the plasma immunoreactive insulin (IRI) concentration as a surrogate marker of insulin resistance or by the minimal model technique [2].
The plasma IRI concentration correlates only moderately to insulin sensitivity when measured with the gold standard euglycaemic insulin clamp technique [3]. In addition, the role of IRI as a risk factor for CHD has been cast in doubt [4, 5]. Even if IRI is accepted as a marker for cardiovascular disease, it is weak compared with established risk markers [6, 7]. Also, the length of follow-up attenuates the strength of IRI as a risk marker [8]. Further, the strength of various risk factors for CHD may change between middle-aged and elderly patients [9].
Proinsulin, in contrast to specific insulin, was recently shown to be a long-term predictor of CHD in middle-aged men in the UK [10] and in Sweden [11]. Also, in studies with a shorter follow-up, proinsulin predicts myocardial infarction [12] and first-ever stroke [13].
The aim of this study was to investigate, using data from the ULSAM cohort (Uppsala Longitudinal Study of Adult Men) with baseline at age 70, whether insulin-mediated glucose uptake measured with the euglycaemic insulin clamp [14], intact and 32–33 split proinsulin and true insulin measured by specific methods [15] are predictive of CHD in elderly males with up to 10 years of follow-up, and whether such associations are influenced by conventional risk factors.
Subjects, materials and methods
Study population
In 1970, all men born from 1920 to 1924 and residing in Uppsala were invited to a health survey, in which 82% (n=2,322) participated [16]. After 20 years, at the age of 70, they were invited for re-investigation, which formed the baseline of the present study, comprising 1,221 of the 1,681 men who were still alive (73%) [17]. Complete data from the baseline investigation at age 70 years were available from 1,166 subjects.
In order to select subjects free from cardiovascular disease (CVD) at baseline, 351 men were excluded due to the presence of: (1) prior myocardial infarction or angina pectoris; (2) Q or QS-complexes or left bundle branch block (Minnesota codes 1.1–1.3 or 7.1, respectively) in the baseline ECG-registration; and (3) previous CVD (International Classification of Diseases, 9th revision [ICD-9] codes:390–459, equivalent to 10th revision [ICD-10] codes I00–I99) or incident CVD up to 1 year after baseline (n=4) to avoid subclinical CVD or current treatment with nitrates or cardiac glycosides. Subjects identified with diabetes at baseline were excluded, as fasting concentrations of insulin are to a varying extent affected by the diabetic state, with elevated concentrations driven by insulin resistance in early type 2 diabetes or by insulinopenia, due to later beta cell failure. After these exclusions, the main analysis in total comprised 815 subjects.
Subjects’ medical histories and ongoing current pharmacological treatments were collected using the original protocol questionnaire [16]. CHD mortality and morbidity data were collected from the official Swedish registries held by The Centre for Epidemiology, National Board of Health and Welfare in Sweden.
Informed consent and ethics committee approval
The Ethics Committee of the Faculty of Medicine at Uppsala University approved the study. Written informed consent was obtained from all subjects.
Follow-up data
CHD was defined on the basis of cause of death recorded in the Cause of Death Registry, or for patients first hospitalised for CHD on the basis of diagnoses (ICD-9 codes:410–414, ICD-10 codes I20–25) recorded in the Hospital-Discharge Registry (censor date December 31, 2001). CHD morbidity, defined by combining data from the Cause of Death Registry and the Hospital Discharge Registry, is an efficient, validated alternative to revised hospital discharge notes and death certificates [18, 19]. No subject was lost to follow-up due to missing registry data.
Euglyacemic insulin clamp
For measurement of insulin sensitivity [14], insulin was infused at a constant rate of 56 mU·min−1·m−2 calculated to achieve nearly complete suppression of hepatic glucose output. The target level of plasma glucose (measured every 5th minute during the 2-h clamp) was 5.1 mmol/l. Median was 5.1 mmol/l, 5th percentile 5.0 mmol/l, 95% percentile 5.4 mmol/l and mean (±SD) 5.2 (±1.3) mmol/l. The insulin sensitivity index (Si) was calculated as glucose disposal rate (glucose infused in mg·min−1·kg body weight−1) divided by the mean plasma insulin concentration per 100 mU/l during the last 60 min of the 2-h euglycaemic insulin clamp.
Baseline characteristics
Blood samples were drawn in the morning after an overnight fast. The plasma concentrations of intact proinsulin and 32–33 split proinsulin were analysed using the two-site immunometric assay technique [15] and concentrations of specific insulin by the Access Immunoassay System (Sanofi Pasteur Diagnostics), blinded for outcome, at the Department of Clinical Biochemistry, Addenbrooke’s Hospital, Cambridge, UK. Assays are highly specific and cross reactivity was less than 1% with insulin in the intact proinsulin assay [15]. IRI was determined by the Phadebas insulin test (Pharmacia, Uppsala, Sweden) [20].
Type 2 diabetes mellitus and IGT were defined according to the WHO 1999 criteria [21] using a 75-g OGTT or the use of oral hypoglycaemic agents. Fasting concentrations of plasma glucose and serum cholesterol, weight, height, BMI and an ECG, supine systolic and diastolic blood pressures were measured under standardised conditions [17, 20]. Smoking status was taken from the questionnaire.
Statistical analyses
Skewed variables were log-transformed to achieve normal distribution. Normally distributed variables were used in all statistical analyses. The statistical software package STATA 6.0 for PC (STATA, College Station, TX, USA) was used. All tests were two-tailed and a p-value of less than 0.05 was considered significant. Associations between baseline variables were analysed using Pearson product moment correlations. In the prospective analyses, Cox’s proportional hazard regression analyses were used. Hazard ratios (HRs) with two-tailed 95% CIs were investigated for a one standard deviation increase in a continuous variable and for a one step increase in the dichotomous variable smoking, to determine the magnitude of the relationship to, and the statistical significance of the predictors of the defined outcome. Kaplan–Meier plots were performed to confirm proportionality of hazards. No violations of the proportional assumption were found using Schoenfeld’s residuals in a linear correlation test for each Cox model presented. In the multivariate CHD models, adjustments were made for the following risk factors: serum cholesterol, systolic blood pressure, fasting plasma glucose, BMI and smoking.
Results
Baseline clinical characteristics at age 70 and standardised crude HRs for a first CHD event during follow-up are shown in Table 1. The subjects had a median follow-up time of 7.9 years (maximum 10.4 years), with a total of 5,972 person–years at risk (PYAR). During follow-up, 126 of 815 subjects (rate 2.11/100 PYAR) had a CHD event, of whom 51 died. The “overlap” of CHD cases between this study and our previous study of the ULSAM-cohort [11] with baseline at age 50 instead of age 70 as in the present study was only 12 out of 126 cases (9.5%). IGT (n= 214/815) did not predict CHD (HR:1.18; 95% CI:0.82–1.69; p=0.36)
Si, intact and 32–33 split proinsulin, serum cholesterol, smoking, systolic blood pressure, fasting glucose and BMI were all associated with a subsequent CHD event in the univariate analyses (Table 1), whereas specific insulin, IRI or diastolic blood pressure were not.
Unadjusted Kaplan–Meier survival curves showed that the risk of CHD was higher for men in the lowest tertile compared to men in the highest tertile of Si (<3.6 vs >5.8, p<0.001; Fig. 1a). For plasma proinsulin concentrations, the risk of CHD was higher in the highest tertile compared to the lowest tertile (>8.1 pmol/l vs <4.8 pmol/l, p<0.001; Fig. 1b).
Kaplan–Meier survival curves for subjects free from subsequent CHD events during 10.4 years of follow-up, for a tertiles of insulin sensitivity index (Si), and b tertiles of intact proinsulin at baseline. The risk of CHD was significantly higher for men in the lowest tertile (T1) of Si than for those in the highest tertile (T3), (Si <3.6 vs >5.8, p<0.001). Similarly, the risk of CHD was significantly higher for men in the highest tertile (T3) of proinsulin concentration than for those in the lowest tertile (T1), (proinsulin >8.1 vs <4.8 pmol/l, p<0.001)
The association between Si and CHD, adjusted for serum cholesterol, systolic blood pressure, fasting glucose, BMI and smoking in multivariate analysis, showed that a 1-SD increase in Si decreased the risk for a CHD event by 18% (Table 2, model 1).
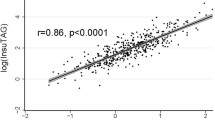
In similar multivariate models, intact proinsulin predicted CHD independently of serum cholesterol, systolic blood pressure, fasting glucose, BMI and smoking (Table 2, model 2), in contrast to 32–33 split proinsulin or specific insulin or IRI (Table 2, models 3, 4 and 5). Combined models including Si and proinsulin or Si and insulin, where the associations for both with CHD became non-significant, were not valid due to co-linearity between Si and proinsulin or Si and insulin. The cross-sectional association with Si was stronger for plasma values of proinsulin (r=−0.51, p<0.001) and insulin (r=−0.62, p<0.001) than the association between early insulin response at an OGTT and proinsulin (r=0.21, p<0.001) or insulin (r=0.36, p<0.001).
Discussion
A low insulin-mediated glucose uptake measured by the euglycaemic insulin clamp technique [14] predicted subsequent CHD over a follow-up period up to 10 years in this population-based cohort study of 70-year old men and thus suggested that insulin resistance makes a major contribution to mortality and morbidity also in the elderly. The risk of subsequent CHD was independent of serum cholesterol, systolic blood pressure, fasting glucose, BMI and smoking, in contrast to a similar analysis of specific insulin or IRI, which are commonly used as surrogate markers for insulin sensitivity. Like insulin-mediated glucose uptake, serum proinsulin was independent of the conventional risk factors named above in predicting CHD.
The observation that decreased insulin-mediated glucose disposal, in contrast to specific insulin concentrations, predicted subsequent CHD indicates that the link between atherosclerosis and insulin resistance is more closely associated with impaired insulin action than with the compensatory increase of plasma insulin, which has been suggested to be atherogenic [22]. The weak association between plasma insulin and CHD is supported by evidence from 25 prospective epidemiological studies [6] and, for subjects with type 2 diabetes, evidence from the UKPDS [23]. In a meta-analysis [7] of 12 large-scale longitudinal studies, it was found that the association between IRI and CHD was modified by the type of insulin assay used. Recent studies using the homeostasis model assessment of insulin resistance (HOMA-IR) index as a surrogate marker of insulin sensitivity have also reported conflicting results [24, 25]. The variation in HOMA-IR is explained to a great extent by the variation in insulin [24]. In contrast to most previous epidemiological studies, which have measured IRI with assays that cross-react with proinsulin, our study avoided this problem by using assays specific for insulin and proinsulin.
Defective insulin action assessed by the euglycaemic insulin clamp is associated, more strongly than plasma insulin, with a well-established cluster of abnormalities, i.e. type 2 diabetes mellitus or IGT, hypertension, dyslipidaemia, and central obesity, which together comprise the insulin resistance syndrome [5]. Another abnormality that may play a role in promoting an increased risk of CHD is the minor elevation of plasma glucose that follows impaired insulin action and underlies hypersecretion of insulin and its propeptides [26]. Also strongly associated with insulin resistance are elevated plasma NEFA, which aggravate the insulin-resistant state both in skeletal muscle and in the liver, and also have direct vascular effects like promoting endothelial dysfunction [27, 28] and elevating blood pressure [29].
Consistent with previous studies in middle-aged men [10, 11, 30], plasma proinsulin was a stronger predictor of CHD than insulin. High plasma proinsulin concentrations are associated with coronary artery atherosclerosis [31] and with increased intimal media thickness in the common carotid artery [32]. In clinical trials with human proinsulin, a several-fold increase was found in cardiovascular events in comparison with human insulin [33], which suggested that thrombo-embolic mechanisms had been activated [33]. In vitro, proinsulin stimulates production of plasminogen activator inhibitor-1 (PAI-1) [34, 35], a putative link between athero-thrombosis and elevated proinsulin concentrations preceding the onset of CHD [36]. The association between proinsulin and atherosclerosis in the common carotid artery also became attenuated by adjustment for PAI-1 in one study [32]. These findings suggest that proinsulin plays some role in biological mechanisms involving atherothrombosis. Another possibility suggested is that proinsulin-like molecules have actions via a proinsulin receptor [37]. With these data in mind, we have not used the term risk factor to describe the observed associations, but instead have chosen the term predictor (equivalent to risk marker) for proinsulin, as published observational studies [10–13] and the present study do not provide sufficient evidence to support a causal linkage.
Elevated plasma proinsulin, an indicator of beta cell hypersecretion, showed a strong association with the degree of insulin resistance. Both were found to be predictors of CHD in this cohort, but when included in the same model, their predictive capacity was weakened. Proinsulin, as a marker of insulin resistance and Si may therefore partly reflect different aspects of insulin resistance. Proinsulin and insulin concentrations are measured in the fasting state and could thus reflect hepatic insulin resistance to a greater extent than insulin-mediated glucose uptake during a euglycaemic insulin clamp, which mainly measures skeletal muscle glucose uptake at an insulin level at which hepatic glucose production is suppressed in the majority of subjects.
Type 2 diabetes mellitus was associated with CHD, in contrast to IGT, which is consistent with previous findings in elderly subjects in Finland [9]. Subjects with diabetes have an increased risk of CHD [38] and have elevated plasma proinsulin [39]. By excluding prevalent diabetes at baseline in our main analysis, we avoided confounding by co-morbidity of the relationship between proinsulin and CHD. The present demonstration that elevated serum proinsulin is a predictor of CHD also in the elderly non-diabetic population extends our previous report in middle-aged men [11] and one report on proinsulin as a predictor of CHD in middle-aged subjects in Britain [10].
At age 70, subjects with the insulin resistance syndrome [5] from the original cohort with baseline at age 50 and examined between 1970 and 1973 are likely to have escaped follow-up due to increased cardiovascular mortality before they were invited to the re-investigations that formed the baseline of the present study at age 70. Thus, the magnitude of the observed associations between insulin resistance, proinsulin and CHD are lower at age 70 than in middle-aged subjects [11].
The present study is unable to answer the question of whether the prediction of CHD risk can also be applied to women. However, in another study of elderly subjects without type 2 diabetes and which included men and women, proinsulin was more strongly and consistently associated with CHD than specific insulin [40].
We conclude that insulin resistance determined by the euglycaemic insulin clamp in elderly men is a predictor of CHD, independently of conventional cardiovascular risk factors. Further, proinsulin provides better prediction of CHD than insulin as a surrogate risk marker for insulin resistance.
Abbreviations
- CVD:
-
cardiovascular disease
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- HR:
-
Hazard ratio
- IRI:
-
immunoreactive insulin
- PAI-1:
-
Plasminogen activator inhibitor-1
- PYAR:
-
person years at risk
- Si :
-
Insulin sensitivity index
References
Beckman JA, Creager MA, Libby P (2002) Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA 287:2570–2581
Howard G, O’Leary DH, Zaccaro D et al (1996) Insulin sensitivity and atherosclerosis. The insulin resistance atherosclerosis study (IRAS) investigators. Circulation 93:1809–1817
Laakso M (1993) How good a marker is insulin level for insulin resistance? Am J Epidemiol 137:959–965
Despres JP, Lamarche B, Mauriege P et al (1996) Hyperinsulinemia as an independent risk factor for ischemic heart disease. N Engl J Med 334:952–957
Reaven GM, Laws A (1994) Insulin resistance, compensatory hyperinsulinaemia, and coronary heart disease. Diabetologia 37:948–952
Wingard DL, Barrett-Connor EL, Ferrara A (1995) Is insulin really a heart disease risk factor? Diabetes Care 18:1299–1304
Ruige JB, Assendelft WJ, Dekker JM, Kostense PJ, Heine RJ, Bouter LM (1998) Insulin and risk of cardiovascular disease: a meta-analysis. Circulation 97:996–1001
Pyorala M, Miettinen H, Laakso M, Pyorala K (1998) Hyperinsulinemia predicts coronary heart disease risk in healthy middle-aged men: the 22-year follow-up results of the Helsinki policemen study. Circulation 98:398–404
Kuusisto J, Mykkanen L, Pyorala K, Laakso M (1994) NIDDM and its metabolic control predict coronary heart disease in elderly subjects. Diabetes 43:960–967
Yudkin JS, May M, Elwood P, Yarnell JW, Greenwood R, Davey Smith G (2002) Concentrations of proinsulin-like molecules predict coronary heart disease risk independently of insulin: prospective data from the Caerphilly study. Diabetologia 45:327–336
Zethelius B, Byberg L, Hales CN, Lithell H, Berne C (2002) Proinsulin is an independent predictor of coronary heart disease: report from a 27-year follow-up study. Circulation 105:2153–2158
Lindahl B, Dinesen B, Eliasson M et al (1999) High proinsulin concentration precedes acute myocardial infarction in a nondiabetic population. Metabolism 48:1197–1202
Lindahl B, Dinesen B, Eliasson M, Roder M, Hallmans G, Stegmayr B (2000) High proinsulin levels precede first-ever stroke in a nondiabetic population. Stroke 31:2936–2941
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237:E214–E223
Sobey WJ, Beer SF, Carrington CA, Clark PMS, Hales CN (1989) Sensitive and specific two-site immunoradiometric assays for human insulin, proinsulin, 65–66 split and 32–33 split proinsulins. Biochem J 260:535–541
Hedstrand H (1975) A study of middle-aged men with particular reference to risk factors for cardiovascular disease. Uppsala J Med Sci 80(Suppl 19):1–61
Byberg L, McKeigue PM, Zethelius B, Lithell HO (2000) Birth weight and the insulin resistance syndrome: association of low birth weight with truncal obesity and raised plasminogen activator inhibitor-1 but not with abdominal obesity or plasma lipid disturbances. Diabetologia 43:54–60
Merlo J, Lindblad U, Pessah-Rasmussen H, et al (2000) Comparison of different procedures to identify probable cases of myocardial infarction and stroke in two Swedish prospective cohort studies using local and national routine registers. Eur J Epidemiol 16:235–243
Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A (1994) Myocardial infarction and coronary deaths in the World Health Organization MONICA project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation 90:583–612
Zethelius B, Hales CN, Lithell HO, Berne C (2004) Insulin resistance, impaired early insulin response, and insulin propeptides as predictors of the development of type 2 diabetes: a population-based, 7-year follow-up study in 70-year-old men. Diabetes Care 27:1433–1438
WHO (1999) Definition, diagnosis and classification of diabetes mellitus and its Complications: report of a WHO consultation. World Health Organization: Geneva. WHO/NCD/NCS/99.2
Stout RW (1996) Hyperinsulinemia and atherosclerosis. Diabetes 45(Suppl 3):S45–S46
Adler AI, Neil HA, Manley SE, Holman RR, Turner RC (1999) Hyperglycemia and hyperinsulinemia at diagnosis of diabetes and their association with subsequent cardiovascular disease in the United Kingdom prospective diabetes study (UKPDS 47). Am Heart J 138:353–359
Hanley AJ, Williams K, Stern MP, Haffner SM (2002) Homeostasis model assessment of insulin resistance in relation to the incidence of cardiovascular disease: the San Antonio heart study. Diabetes Care 25:1177–1184
Resnick HE, Jones K, Ruotolo G et al (2003) Insulin resistance, the metabolic syndrome, and risk of incident cardiovascular disease in nondiabetic American Indians: the strong heart study. Diabetes Care 26:861–867
Coutinho M, Gerstein HC, Wang Y, Yusuf S (1999) The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care 22:233–240
Boden G (1997) Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes 46:3–10
Steinberg HO, Chaker H, Leaming R, Johnson A, Brechtel G, Baron AD (1996) Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J Clin Invest 97:2601–2610
Salonen JT, Lakka TA, Lakka HM, Valkonen VP, Everson SA, Kaplan GA (1998) Hyperinsulinemia is associated with the incidence of hypertension and dyslipidemia in middle-aged men. Diabetes 47:270–275
Yudkin JS (2002) Increased proinsulin concentrations and excess risk of coronary heart disease in patients with diabetes and prediabetes. Circulation 106:e202
Bavenholm P, Proudler A, Tornvall P et al (1995) Insulin, intact and split proinsulin, and coronary artery disease in young men. Circulation 92:1422–1429
Haffner SM, D’Agostino R, Mykkanen L et al (1998) Proinsulin and insulin concentrations in relation to carotid wall thickness: Insulin Resistance Atherosclerosis Study. Stroke 29:1498–1503
Galloway JA, Hooper SA, Spradlin CT et al (1992) Biosynthetic human proinsulin. Review of chemistry, in vitro and in vivo receptor binding, animal and human pharmacology studies, and clinical trial experience. Diabetes Care 15:666–692
Nordt TK, Schneider DJ, Sobel BE (1994) Augmentation of the synthesis of plasminogen activator inhibitor type-1 by precursors of insulin. A potential risk factor for vascular disease. Circulation 89:321–330
Festa A, D. Agostino R J, Mykkanen L et al (1999) Relative contribution of insulin and its precursors to fibrinogen and PAI-1 in a large population with different states of glucose tolerance. The insulin resistance atherosclerosis study (IRAS). Arterioscler Thromb Vasc Biol 19:562–568
Kohler HP, Grant PJ (2000) Plasminogen-activator inhibitor type 1 and coronary artery disease. N Engl J Med 342:1792–1801
Jehle PM, Lutz MP, Fussgaenger RD (1996) High affinity binding sites for proinsulin in human IM-9 lymphoblasts. Diabetologia 39:421–432
Khaw KT, Wareham N, Luben R et al (2001) Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ 322:15–28
Temple RC, Carrington CA, Luzio SD et al (1989) Insulin deficiency in non-insulin-dependent diabetes. Lancet 1:293–295
Oh JY, Barrett-Connor E, Wedick NM (2002) Sex differences in the association between proinsulin and intact insulin with coronary heart disease in nondiabetic older adults: the Rancho Bernardo study. Circulation 105:1311–1316
Acknowledgements
This work was supported by research grants from the Swedish Medical Research Council No. 5446, Medical Research Council UK, Foundation for Geriatric Research, Uppsala Geriatric Fund, Ernfors Fund for Diabetes Research, “Förenade Liv” Mutual Group Life Insurance Company, The Swedish Diabetes Association, Thureus Foundation and Uppsala University. We thank the technical staff of the Department of Clinical Biochemistry, Addenbrooke’s Hospital for the measurements of specific insulin, intact and 32–33-split proinsulin, and Uppsala Clinical Research Centre for excellent statistical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zethelius, B., Lithell, H., Hales, C.N. et al. Insulin sensitivity, proinsulin and insulin as predictors of coronary heart disease. A population-based 10-year, follow-up study in 70-year old men using the euglycaemic insulin clamp. Diabetologia 48, 862–867 (2005). https://doi.org/10.1007/s00125-005-1711-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1711-9