Early psychosis for the non-specialist doctor
BMJ 2017; 357 doi: https://doi.org/10.1136/bmj.j4578 (Published 08 November 2017) Cite this as: BMJ 2017;357:j4578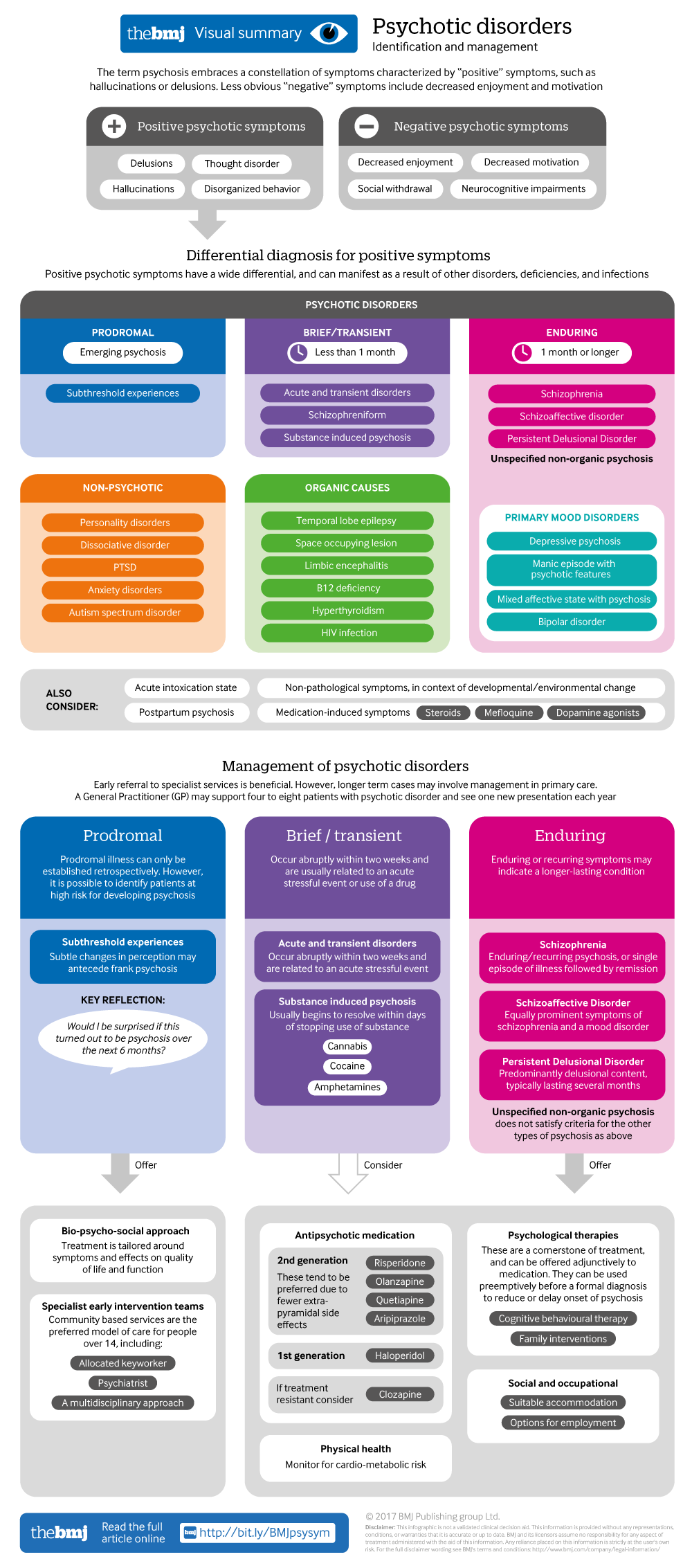
Visual summary available
Click here for an overview of identification and management of psychotic disorders.
- Musa Basseer Sami, MRC clinical research training fellow, honorary specialist registrar1 2,
- David Shiers, former GP, honorary reader in early psychosis3,
- Saqib Latif, clinical lead & consultant child and adolescent psychiatrist4,
- Sagnik Bhattacharyya, reader in translational neuroscience and psychiatry, consultant psychiatrist1 5
- 1Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London SE5 8AF, UK
- 2South London and Maudsley NHS Foundation Trust, London
- 3Manchester University, Manchester, UK
- 4Kent and Medway Children & Young People Services, Sussex Partnership NHS Foundation Trust, Broadstairs, UK
- 5Lambeth Early Onset Inpatient Unit, Lambeth Hospital South London and Maudsley NHS Foundation Trust, London
- Correspondence to: S Bhattacharryya sagnik.2.bhattacharyya{at}kcl.ac.uk, M B Sami musa.sami{at}kcl.ac.uk
What you need to know
Psychosis can be a frightening and bewildering experience for both patients and families. Early proactive support and intervention improves clinical outcomes, avoids costly and traumatic hospital admissions, and is preferred by patients and their families
Have a low threshold for referral for specialist assessment if you suspect psychosis or prodromal illness
People with psychosis face a mortality gap of 10-15 years, mainly from physical comorbidities, especially cardiovascular disease. Identify and treat modifiable risks for cardiovascular disease and type 2 diabetes
A general practitioner may support four to eight patients with psychotic disorder and see one new presentation each year.12 Other non-specialist doctors will encounter patients presenting to an emergency department or complicating comorbid illness.
Psychosis often emerges for the first time in adolescence and young adulthood.3 In around four out of five patients symptoms remit, but most experience relapses and further difficulties.4 The first two to five years of psychosis are considered a critical period for intervening to improve long term outcome.567 The non-specialist plays a key role in early identification. The challenge is to identify a relatively rare but serious disorder and distinguish this from more common but less severe disorders, occurring in a typically young population experiencing developmental and often stressful transitions.
Methods
We searched the Medline database over 10 years (1 January 2007 to 31 January 2017) for review articles on “early psychotic illness” or “early psychosis.” This yielded 779 including Narrative and Systematic Reviews and Meta-analyses. 125 articles were reviewed for relevance and methodology and analysis of data.
What is psychosis?
Fig 1 Where the soft winds blow by Bryan Charnley (1949-1991), who had schizophrenia (www.bryancharnley.info). ©The estate of Bryan Charnley, reproduced with permission
The term psychosis embraces a constellation of symptoms characterised by hallucinations, delusions, or disorganised behaviour or thought (“positive …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £173 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£38 / $45 / €42 (excludes VAT)
You can download a PDF version for your personal record.
