Low back pain and sciatica: summary of NICE guidance
BMJ 2017; 356 doi: https://doi.org/10.1136/bmj.i6748 (Published 06 January 2017) Cite this as: BMJ 2017;356:i6748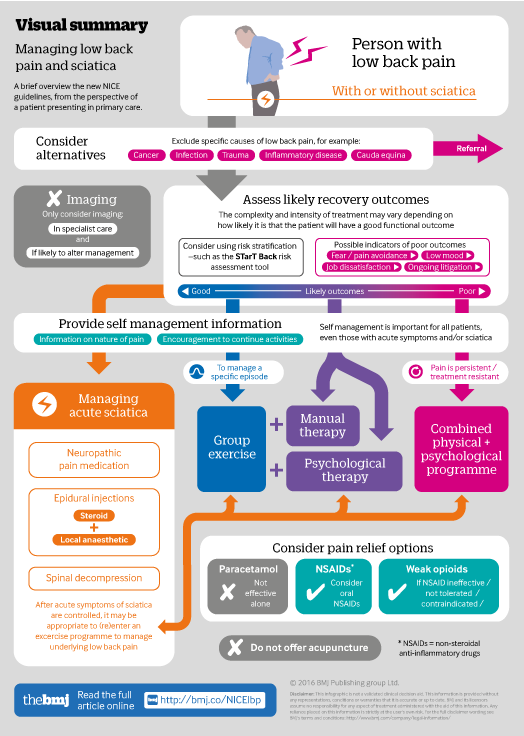
Infographic available
Click here for a visual overview of assessment and management for those with low back pain and/or sciatica.
- Ian A Bernstein, musculoskeletal physician and general practitioner1,
- Qudsia Malik, senior research fellow2,
- Serena Carville, associate director2,
- Stephen Ward, guideline development group chair, consultant pain physician3
- 1London North West Healthcare NHS Trust and Gordon House Surgery, London, UK
- 2National Guideline Centre, Royal College of Physicians, London NW1 4LE, UK
- 3Department of Pain Medicine, Brighton and Sussex University Hospitals NHS Trust, Brighton, UK
- Correspondence to: I A Bernstein ian.bernstein@nhs.net
What you need to know
Consider risk stratification (such as with the STarT Back tool) to target more intensive support at initial presentation for those less likely to recover quickly
Consider exercises such as stretching, strengthening, aerobic, yoga, or Tai Chi in a group setting for all patients with low back pain and sciatica as the main component of non-invasive treatment. Manual therapy and psychological approaches should be recommended only alongside an exercise programme, while acupuncture or electrotherapies should not be recommended
Consider a short course of non-steroidal anti-inflammatory drugs (NSAIDs), or a weak opioid where an NSAID is ineffective or poorly tolerated, and do not offer paracetamol alone for low back pain; and consider neuropathic drugs such as gabapentin and epidural steroids for sciatica
Low back pain is the leading cause of long term disability worldwide.1 The lifetime incidence of low back pain is 58-84%,2 and 11% of men and 16% of women have chronic low back pain.3 Back pain accounts for 7% of GP consultations and results in the loss of 4.1 million working days a year.2 More than 30% of people still have clinically significant symptoms after a year after onset of sciatica.4
This guideline replaces the National Institute for Health and Care Excellence (NICE) guideline on early management of low back pain in adults (2009) and expands its remit. It summarises the updated recommendations from NICE for the assessment and management of low back pain and sciatica.5 For a visual summary, please see infographic. It is intended to overcome patchy commissioning of back pain pathways and pain management programmes6 and poor implementation due to clinicians’ beliefs that previous recommendations were constraining clinical practice.7
Recommendations
NICE recommendations are based on systematic reviews of best available evidence and explicit consideration of cost effectiveness. When minimal evidence …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £173 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£38 / $45 / €42 (excludes VAT)
You can download a PDF version for your personal record.
